Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
Ebixa 10 mg film-coated tablets
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each film-coated tablet contains 10 mg of memantine hydrochloride equivalent to 8.31 mg
memantine.
For a full list of excipients, see section 6.1.
Film-coated tablets.
Pale yellow to yellow, oval shaped film-coated tablet with breaking line and engravings “1 0” on one
side and “M M” on the other side
The tablet can be divided into equal halves.
4.1 Therapeuticindications
Treatment of patients with moderate to severe Alzheimer’s disease.
4.2 Posology and method of administration
Treatment should be initiated and supervised by a physician experienced in the diagnosis and
treatment of Alzheimer’s dementia. Therapy should only be started if a caregiver is available who will
regularly monitor the intake of the medicinal product by the patient. Diagnosis should be made
according to current guidelines.
Ebixa should be administered once a day and should be taken at the same time every day. The film-
coated tablets can be taken with or without food.
The maximum daily dose is 20 mg per day. In order to reduce the risk of undesirable effects, the
maintenance dose is achieved by upward titration of 5 mg per week over the first 3 weeks as follows:
Week 1 (day 1-7):
The patient should take half a 10 mg film-coated tablet (5 mg) per day for 7 days.
Week 2 (day 8-14):
The patient should take one 10 mg film-coated tablet (10 mg) per day for 7 days.
Week 3 (day 15-21):
The patient should take one and a half 10 mg film-coated tablet (15 mg) per day for 7 days.
From Week 4 on:
The patient should take two 10 mg film-coated tablets (20 mg) per day.
The recommended maintenance dose is 20 mg per day.
Elderly:
On the basis of the clinical studies, the recommended dose for patients over the age of 65
years is 20 mg per day (two 10 mg film-coated tablets once a day) as described above.
Children and adolescents:
Ebixa is not recommended for use in children below 18 years due to a lack
of data on safety and efficacy.
Renal impairment:
In patients with mildly impaired renal function (creatinine clearance 50 – 80
ml/min) no dose adjustment is required. In patients with moderate renal impairment (creatinine
clearance 30 - 49 ml/min) daily dose should be 10 mg per day. If tolerated well after at least 7 days of
treatment, the dose could be increased up to 20 mg/day according to standard titration scheme. In
patients with severe renal impairment (creatinine clearance 5 – 29 ml/min) daily dose should be 10 mg
per day
.
Hepatic impairment:
In patients with mild or moderate hepatic impaired function (Child-Pugh A and
Child-Pugh B), no dose adjustment is needed. No data on the use of memantine in patients with severe
hepatic impairment are available. Administration of Ebixa is not recommended in patients with severe
hepatic impairment.
Hypersensitivity to the active substance or to any of the excipients.
4.4 Special warnings and precautions for use
Caution is recommended in patients with epilepsy, former history of convulsions or patients with
predisposing factors for epilepsy.
Concomitant use of N-methyl-D-aspartate(NMDA)-antagonists such as amantadine, ketamine or
dextromethorphan should be avoided. These compounds act at the same receptor system as
memantine, and therefore adverse reactions (mainly central nervous system (CNS)-related) may be
more frequent or more pronounced (see also section 4.5).
Some factors that may raise urine pH (see section 5.2 “Elimination”) may necessitate careful
monitoring of the patient. These factors include drastic changes in diet, e.g. from a carnivore to a
vegetarian diet, or a massive ingestion of alkalising gastric buffers. Also, urine pH may be elevated by
states of renal tubulary acidosis (RTA) or severe infections of the urinary tract with
Proteus bacteria
.
In most clinical trials, patients with recent myocardial infarction, uncompensated congestive heart
failure (NYHA III-IV), or uncontrolled hypertension were excluded. As a consequence, only limited
data are available and patients with these conditions should be closely supervised.
4.5 Interaction with other medicinal products and other forms of interaction
Due to the pharmacological effects and the mechanism of action of memantine the following
interactions may occur:
The mode of action suggests that the effects of L-dopa, dopaminergic agonists, and
anticholinergics may be enhanced by concomitant treatment with NMDA-antagonists such as
memantine. The effects of barbiturates and neuroleptics may be reduced. Concomitant
administration of memantine with the antispasmodic agents, dantrolene or baclofen, can modify
their effects and a dose adjustment may be necessary.
Concomitant use of memantine and amantadine should be avoided, owing to the risk of
pharmacotoxic psychosis. Both compounds are chemically related NMDA-antagonists. The
same may be true for ketamine and dextromethorphan (see also section 4.4). There is one
published case report on a possible risk also for the combination of memantine and phenytoin.
Other active substances such as cimetidine, ranitidine, procainamide, quinidine, quinine and
nicotine that use the same renal cationic transport system as amantadine may also possibly
interact with memantine leading to a potential risk of increased plasma levels.
There may be a possibility of reduced serum level of hydrochlorothiazide (HCT) when
memantine is co-administered with HCT or any combination with HCT.
In post-marketing experience, isolated cases with international normalized ratio (INR) increases
have been reported in patients concomitantly treated with warfarin. Although no causal
relationship has been established, close monitoring of prothrombin time or INR is advisable for
patients concomitantly treated with oral anticoagulants.
In single-dose pharmacokinetic (PK) studies in young healthy subjects, no relevant active substance-
active substance interaction of memantine with glyburide/metformin or donepezil was observed.
In a clinical study in young healthy subjects, no relevant effect of memantine on the pharmacokinetics
of galantamine was observed.
Memantine did not inhibit CYP 1A2, 2A6, 2C9, 2D6, 2E1, 3A, flavin containing monooxygenase,
epoxide hydrolase or sulphation
in vitro
.
4.6 Pregnancy and lactation
For memantine, no clinical data on exposed pregnancies are available. Animal studies indicate a
potential for reducing intrauterine growth at exposure levels, which are identical or slightly higher
than at human exposure (see section 5.3). The potential risk for humans is unknown. Memantine
should not be used during pregnancy unless clearly necessary.
It is not known whether memantine is excreted in human breast milk but, taking into consideration the
lipophilicity of the substance, this probably occurs. Women taking memantine should not breast-feed.
4.7 Effects on ability to drive and use machines
Moderate to severe Alzheimer’s disease usually causes impairment of driving performance and
compromises the ability to use machinery. Furthermore, Ebixa has minor to moderate influence on the
ability to drive and use machines such that outpatients should be warned to take special care.
In clinical trials in mild to severe dementia, involving 1,784 patients treated with Ebixa and 1,595
patients treated with placebo, the overall incidence rate of adverse reactions with Ebixa did not differ
from those with placebo; the adverse reactions were usually mild to moderate in severity. The most
frequently occurring adverse reactions with a higher incidence in the Ebixa group than in the placebo
group were dizziness (6.3% vs 5.6%, respectively), headache (5.2% vs 3.9%), constipation (4.6% vs
2.6%), somnolence (3.4% vs 2.2%) and hypertension (4.1% vs 2.8%).
The following Adverse Reactions listed in the Table below have been accumulated in clinical studies
with Ebixa and since its introduction in the market. Within each frequency grouping, undesirable
effects are presented in order of decreasing seriousness.
Adverse reactions are ranked according to system organ class, using the following convention: very
common (≥1/10), common (≥1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥1/10,000 to <
1/1,000), very rare (< 1/10,000), not known (cannot be estimated from the available data).
Infections and infestations
Venous
thrombosis/thromboembolism
Respiratory, thoracic and mediastinal
disorders
Gastrointestinal disorders
General disorders and administration
site conditions
Uncommon Fatigue
1
Hallucinations have mainly been observed in patients with severe Alzheimer´s disease.
2
Isolated cases reported in post-marketing experience.
Alzheimer’s disease has been associated with depression, suicidal ideation and suicide. In post-
marketing experience these events have been reported in patients treated with Ebixa.
Only limited experience with overdose is available from clinical studies and post-marketing
experience.
Symptoms:
Relative large overdoses (200 mg and 105 mg/day for 3 days, respectively) have been
associated with either only symptoms of tiredness, weakness and/or diarrhoea or no symptoms. In the
overdose cases below 140 mg or unknown dose the patients revealed symptoms from central nervous
system (confusion, drowsiness, somnolence, vertigo, agitation, aggression, hallucination, and gait
disturbance) and/or of gastrointestinal origin (vomiting and diarrhoea).
In the most extreme case of overdose, the patient survived the oral intake of a total of 2000 mg
memantine with effects on the central nervous system (coma for 10 days, and later diplopia and
agitation). The patient received symptomatic treatment and plasmapheresis. The patient recovered
without permanent sequelae.









In another case of a large overdose, the patient also survived and recovered. The patient had received
400 mg memantine orally. The patient experienced central nervous system symptoms such as
restlessness, psychosis, visual hallucinations, proconvulsiveness, somnolence, stupor, and
unconsciousness.
Treatment:
In the event of overdose, treatment should be symptomatic. No specific antidote for
intoxication or overdose is available. Standard clinical procedures to remove active substance material,
e.g. gastric lavage, carbo medicinalis (interruption of potential entero-hepatic recirculation),
acidification of urine, forced diuresis should be used as appropriate.
In case of signs and symptoms of general central nervous system (CNS) overstimulation, careful
symptomatic clinical treatment should be considered.
5. PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamicproperties
Pharmacotherapeutic group: Other Anti-dementia drugs, ATC code: N06DX01.
There is increasing evidence that malfunctioning of glutamatergic neurotransmission, in particular at
NMDA-receptors, contributes to both expression of symptoms and disease progression in
neurodegenerative dementia.
Memantine is a voltage-dependent, moderate-affinity uncompetitive NMDA-receptor antagonist. It
modulates the effects of pathologically elevated tonic levels of glutamate that may lead to neuronal
dysfunction.
Clinical studies:
A pivotal monotherapy study in a population of patients suffering from moderate to
severe Alzheimer’s disease (mini mental state examination (MMSE) total scores at baseline of 3 - 14)
included a total of 252 outpatients. The study showed beneficial effects of memantine treatment in
comparison to placebo at 6 months (observed cases analysis for the clinician´s interview based
impression of change (CIBIC-plus): p=0.025; Alzheimer´s disease cooperative study – activities of
daily living (ADCS-ADLsev): p=0.003; severe impairment battery (SIB): p=0.002).
A pivotal monotherapy study of memantine in the treatment of mild to moderate Alzheimer’s disease
(MMSE total scores at baseline of 10 to 22) included 403 patients. Memantine-treated patients showed
a statistically significantly better effect than placebo-treated patients on the primary endpoints:
Alzheimer´s disease assessment scale (ADAS-cog) (p=0.003) and CIBIC-plus (p=0.004) at week 24
(last observation carried forward (LOCF)). In another monotherapy study in mild to moderate
Alzheimer’s disease a total of 470 patients (MMSE total scores at baseline of 11-23) were randomised.
In the prospectively defined primary analysis statistical significance was not reached at the primary
efficacy endpoint at week 24.
A meta-analysis of patients with moderate to severe Alzheimer’s disease (MMSE total scores < 20)
from the six phase III, placebo-controlled, 6-month studies (including monotherapy studies and studies
with patients on a stable dose of acetylcholinesterase inhibitors) showed that there was a statistically
significant effect in favour of memantine treatment for the cognitive, global, and functional domains.
When patients were identified with concurrent worsening in all three domains, results showed a
statistically significant effect of memantine in preventing worsening, as twice as many placebo-treated
patients as memantine-treated patients showed worsening in all three domains (21% vs. 11%,
p<0.0001).
5.2 Pharmacokineticproperties
Absorption:
Memantine has an absolute bioavailability of approximately 100%. t
max
is between 3 and
8 hours. There is no indication that food influences the absorption of memantine.
Distribution:
Daily doses of 20 mg lead to steady-state plasma concentrations of memantine ranging
from 70 to 150 ng/ml (0.5 - 1 µmol) with large interindividual variations. When daily doses of 5 to
30 mg were administered, a mean cerebrospinal fluid (CSF)/serum ratio of 0.52 was calculated. The
volume of distribution is around 10 l/kg. About 45% of memantine is bound to plasma-proteins.
Biotransformation:
In man, about 80% of the circulating memantine-related material is present as the
parent compound. Main human metabolites are N-3,5-dimethyl-gludantan, the isomeric mixture of 4-
and 6-hydroxy-memantine, and 1-nitroso-3,5-dimethyl-adamantane. None of these metabolites exhibit
NMDA-antagonistic activity. No cytochrome P 450 catalysed metabolism has been detected
in vitro.
In a study using orally administered
14
C-memantine, a mean of 84% of the dose was recovered within
20 days, more than 99% being excreted renally.
Elimination:
Memantine is eliminated in a monoexponential manner with a terminal t
½
of 60 to
100 hours. In volunteers with normal kidney function, total clearance (Cl
tot
) amounts to
170 ml/min/1.73 m² and part of total renal clearance is achieved by tubular secretion.
Renal handling also involves tubular reabsorption, probably mediated by cation transport proteins. The
renal elimination rate of memantine under alkaline urine conditions may be reduced by a factor of 7 to
9 (see section 4.4). Alkalisation of urine may result from drastic changes in diet, e.g. from a carnivore
to a vegetarian diet, or from the massive ingestion of alkalising gastric buffers.
Linearity:
Studies in volunteers have demonstrated linear pharmacokinetics in the dose range of 10 to
40 mg.
Pharmacokinetic/pharmacodynamic relationship:
At a dose of memantine of 20 mg per day the CSF
levels match the k
i
-value (k
i
= inhibition constant) of memantine, which is 0.5 µmol in human frontal
cortex.
5.3 Preclinical safety data
In short term studies in rats, memantine like other NMDA-antagonists have induced neuronal
vacuolisation and necrosis (Olney lesions) only after doses leading to very high peak serum
concentrations. Ataxia and other preclinical signs have preceded the vacuolisation and necrosis. As the
effects have neither been observed in long term studies in rodents nor in non-rodents, the clinical
relevance of these findings is unknown.
Ocular changes were inconsistently observed in repeat dose toxicity studies in rodents and dogs, but
not in monkeys. Specific ophthalmoscopic examinations in clinical studies with memantine did not
disclose any ocular changes.
Phospholipidosis in pulmonary macrophages due to accumulation of memantine in lysosomes was
observed in rodents. This effect is known from other active substances with cationic amphiphilic
properties. There is a possible relationship between this accumulation and the vacuolisation observed
in lungs. This effect was only observed at high doses in rodents. The clinical relevance of these
findings is unknown.
No genotoxicity has been observed following testing of memantine in standard assays. There was no
evidence of any carcinogenicity in life long studies in mice and rats. Memantine was not teratogenic in
rats and rabbits, even at maternally toxic doses, and no adverse effects of memantine were noted on
fertility. In rats, foetal growth reduction was noted at exposure levels, which are identical or slightly
higher than at human exposure.
6. PHARMACEUTICAL PARTICULARS
Tablet core:
Microcrystalline cellulose
Croscarmellose sodium
Colloidal anhydrous silica
Magnesium stearate
Tablet coat:
Hypromellose
Macrogol 400
Titanium dioxide (E 171)
Iron oxide yellow (E 172)
6.4 Special precautions for storage
This medicinal product does not require any special storage conditions.
6.5 Nature and contents of container
Blister packs containing either 7,
10, 14 or 20 tablets per blister strip. Pack sizes of 14, 28, 30, 42, 49 x
1, 50, 56, 56 x 1, 70, 84, 98, 98 x 1, 100, 100 x 1, 112, 980 (10 x 98) or 1000 (20 x 50) tablets are
presented. The pack sizes 49 x 1, 56 x1, 98 x 1 and 100 x 1 film-coated tablets are presented in unit
dose blister
.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
7. MARKETING AUTHORISATION HOLDER
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Denmark
8. MARKETING AUTHORISATION NUMBER(S)
EU/1/02/219/001-003
EU/1/02/219/007-012
EU/1/02/219/014-021
9. DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 15/05/2002
Date of latest renewal: 15/05/2007
10. DATE OF REVISION OF THE TEXT
Detailed information on this product is available on the website of the European Medicines Agency
(EMA) http://www.ema.europa.eu
NAME OF THE MEDICINAL PRODUCT
Ebixa 10 mg/g oral drops, solution.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each activation of the pump (one downward stroke) delivers 0.5 ml (0.5g) of solution containing 5 mg
of memantine hydrochloride equivalent to 4.16 mg of memantine
Excipients:
Each one gram of solution contains 100 mg sorbitol (E420) and 0.5 mg potassium, see
section 4.4.
For a full list of excipients, see section 6.1.
Oral drops, solution.
The solution is clear and colourless to light yellowish.
4.1 Therapeuticindications
Treatment of patients with moderate to severe Alzheimer’s disease.
4.2 Posology and method of administration
Treatment should be initiated and supervised by a physician experienced in the diagnosis and
treatment of Alzheimer’s dementia. Therapy should only be started if a caregiver is available who will
regularly monitor the intake of the medicinal product by the patient. Diagnosis should be made
according to current guidelines.
Ebixa should be taken once daily at the same time each day. The solution can be taken with or without
food. The solution must not be poured or pumped into the mouth directly from the bottle or the pump,
but should be dosed onto a spoon or into a glass of water using the pump.
For detailed instructions on the preparation and handling of the product see section 6.6.
The maximum daily dose is 20 mg once daily. In order to reduce the risk of undesirable effects, the
maintenance dose is achieved by upward titration of 5 mg per week over the first 3 weeks as follows:
Week 1 (day 1-7):
The patient should take 0.5 ml solution (5 mg) equivalent to one downward stroke per day for 7 days.
Week 2 (day 8-14):
The patient should take 1 ml solution (10 mg) equivalent to two downward strokes per day for 7 days.
Week 3 (day 15-21):
The patient should take 1.5 ml solution (15 mg) equivalent to three downward strokes per day for 7 days.
From Week 4 on:
The patient should take 2 ml solution (20 mg) equivalent to four downward strokes once a day.
Maintenance dose
The recommended maintenance dose is 20 mg per day.
Elderly:
On the basis of the clinical studies, the recommended dose for patients over the age of 65
years is 20 mg per day (2 ml solution, equivalent to four downward strokes) as described above.
Children and adolescents:
Ebixa is not recommended for use in children below 18 years due to a lack
of data on safety and efficacy.
Renal impairment:
In patients with mildly impaired renal function (creatinine clearance 50 – 80
ml/min) no dose adjustment is required. In patients with moderate renal impairment (creatinine
clearance 30 - 49 ml/min) daily dose should be 10 mg (1 ml solution, equivalent to two downward
strokes). If tolerated well after at least 7 days of treatment, the dose could be increased up to 20
mg/day according to standard titration scheme. In patients with severe renal impairment (creatinine
clearance 5 – 29 ml/min) daily dose should be 10 mg (1 ml solution, equivalent to two downward
strokes) per day.
Hepatic impairment:
In patients with mild or moderate hepatic impaired function (Child-Pugh A and
Child-Pugh B), no dose adjustment is needed. No data on the use of memantine in patients with severe
hepatic impairment are available. Administration of Ebixa is not recommended in patients with severe
hepatic impairment.
Hypersensitivity to the active substance or to any of the excipients.
4.4 Special warnings and precautions for use
Caution is recommended in patients with epilepsy, former history of convulsions or patients with
predisposing factors for epilepsy.
Concomitant use of other N-methyl-D-aspartate(NMDA)-antagonists such as amantadine, ketamine or
dextromethorphan should be avoided. These compounds act at the same receptor system as
memantine, and therefore adverse reactions (mainly central nervous system (CNS)-related) may be
more frequent or more pronounced (see also section 4.5).
Some factors that may raise urine pH (see section 5.2 “Elimination”) may necessitate careful
monitoring of the patient. These factors include drastic changes in diet, e.g. from a carnivore to a
vegetarian diet, or a massive ingestion of alkalising gastric buffers. Also, urine pH may be elevated by
states of renal tubulary acidosis (RTA) or severe infections of the urinary tract with
Proteus bacteria
.
In most clinical trials, patients with recent myocardial infarction, uncompensated congestive heart
failure (NYHA III-IV), or uncontrolled hypertension were excluded. As a consequence, only limited
data are available and patients with these conditions should be closely supervised.
Excipients:
The oral solution contains sorbitol. Patients with rare hereditary problems of fructose
intolerance should not take this medicine.
4.5 Interaction with other medicinal products and other forms of interaction
Due to the pharmacological effects and the mechanism of action of memantine the following
interactions may occur:
The mode of action suggests that the effects of L-dopa, dopaminergic agonists, and
anticholinergics may be enhanced by concomitant treatment with NMDA-antagonists such as
memantine. The effects of barbiturates and neuroleptics may be reduced. Concomitant
administration of memantine with the antispasmodic agents, dantrolene or baclofen, can modify
their effects and a dose adjustment may be necessary.
Concomitant use of memantine and amantadine should be avoided, owing to the risk of
pharmacotoxic psychosis. Both compounds are chemically related NMDA-antagonists. The
same may be true for ketamine and dextromethorphan (see also section 4.4). There is one
published case report on a possible risk also for the combination of memantine and phenytoin.
Other active substances such as cimetidine, ranitidine, procainamide, quinidine, quinine and
nicotine that use the same renal cationic transport system as amantadine may also possibly
interact with memantine leading to a potential risk of increased plasma levels.
There may be a possibility of reduced serum level of hydrochlorothiazide (HCT) when
memantine is co-administered with HCT or any combination with HCT.
In post-marketing experience, isolated cases with international normalized ratio (INR) increases
have been reported in patients concomitantly treated with warfarin. Although no causal
relationship has been established, close monitoring of prothrombin time or INR is advisable for
patients concomitantly treated with oral anticoagulants.
In single-dose pharmacokinetic (PK) studies in young healthy subjects, no relevant active substance-
active substance interaction of memantine with glyburide/metformin or donepezil was observed.
In a clinical study in young healthy subjects, no relevant effect of memantine on the pharmacokinetics
of galantamine was observed.
Memantine did not inhibit CYP 1A2, 2A6, 2C9, 2D6, 2E1, 3A, flavin containing monooxygenase,
epoxide hydrolase or sulphation
in vitro
.
4.6 Pregnancy and lactation
For memantine, no clinical data on exposed pregnancies are available. Animal studies indicate a
potential for reducing intrauterine growth at exposure levels, which are identical or slightly higher
than at human exposure (see section 5.3). The potential risk for humans is unknown. Memantine
should not be used during pregnancy unless clearly necessary.
It is not known whether memantine is excreted in human breast milk but, taking into consideration the
lipophilicity of the substance, this probably occurs. Women taking memantine should not breast-feed.
4.7 Effects on ability to drive and use machines
Moderate to severe Alzheimer’s disease usually causes impairment of driving performance and
compromises the ability to use machinery. Furthermore, Ebixa has minor or moderate influence on the
ability to drive and use machines such that outpatients should be warned to take special care.
In clinical trials in mild to severe dementia, involving 1,784 patients treated with Ebixa and 1,595
patients treated with placebo, the overall incidence rate of adverse reactions with Ebixa did not differ
from those with placebo; the adverse reactions were usually mild to moderate in severity. The most
frequently occurring adverse reactions with a higher incidence in the Ebixa group than in the placebo
group were dizziness (6.3% vs 5.6%, respectively), headache (5.2% vs 3.9%), constipation (4.6% vs
2.6%), somnolence (3.4% vs 2.2%) and hypertension (4.1% vs 2.8%).
The following Adverse Reactions listed in the Table below have been accumulated in clinical studies
with Ebixa and since its introduction in the market. Within each frequency grouping, undesirable
effects are presented in order of decreasing seriousness.
Adverse reactions are ranked according to system organ class, using the following convention: very
common (≥ 1/10), common (≥1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥1/10,000 to
< 1/1,000), very rare (< 1/10,000), not known (cannot be estimated from the available data).
Infections and infestations
Venous
thrombosis/thromboembolism
Respiratory, thoracic and mediastinal
disorders
Gastrointestinal disorders
General disorders and administration
site conditions
Uncommon Fatigue
1
Hallucinations have mainly been observed in patients with severe Alzheimer´s disease.
2
Isolated cases reported in post-marketing experience.
Alzheimer’s disease has been associated with depression, suicidal ideation and suicide. In post-
marketing experience these events have been reported in patients treated with Ebixa.
Only limited experience with overdose is available from clinical studies and post-marketing
experience.
Symptoms:
Relative large overdoses (200 mg and 105 mg/day for 3 days, respectively) have been
associated with either only symptoms of tiredness, weakness and/or diarrhoea or no symptoms. In the
overdose cases below 140 mg or unknown dose the patients revealed symptoms from central nervous
system (confusion, drowsiness, somnolence, vertigo, agitation, aggression, hallucination and gait
disturbance) and/or of gastrointestinal origin (vomiting and diarrhoea).










In the most extreme case of overdose, the patient survived the oral intake of a total of 2000 mg
memantine with effects on the central nervous system (coma for 10 days, and later diplopia and
agitation). The patient received symptomatic treatment and plasmapheresis. The patient recovered
without permanent sequelae.
In another case of a large overdose, the patient also survived and recovered. The patient had received
400 mg memantine orally. The patient experienced central nervous system symptoms such as
restlessness, psychosis, visual hallucinations, proconvulsiveness, somnolence, stupor, and
unconsciousness.
Treatment:
In the event of overdose, treatment should be symptomatic. No specific antidote for
intoxication or overdose is available. Standard clinical procedures to remove active substance material,
e.g. gastric lavage, carbo medicinalis (interruption of potential entero-hepatic recirculation),
acidification of urine, forced diuresis should be used as appropriate.
In case of signs and symptoms of general central nervous system (CNS) overstimulation, careful
symptomatic clinical treatment should be considered.
5. PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamicproperties
Pharmacotherapeutic group: Other Anti-dementia drugs, ATC code: N06DX01.
There is increasing evidence that malfunctioning of glutamatergic neurotransmission, in particular at
NMDA-receptors, contributes to both expression of symptoms and disease progression in
neurodegenerative dementia.
Memantine is a voltage-dependent, moderate-affinity uncompetitive NMDA-receptor antagonist. It
modulates the effects of pathologically elevated tonic levels of glutamate that may lead to neuronal
dysfunction.
Clinical studies:
A pivotal monotherapy study in a population of patients suffering from moderate to
severe Alzheimer’s disease (mini mental state examination (MMSE) total scores at baseline of 3 - 14)
included a total of 252 outpatients. The study showed beneficial effects of memantine treatment in
comparison to placebo at 6 months (observed cases analysis for the clinican´s interview based
impression of change (CIBIC-plus): p=0.025; Alzheimer´s disease cooperative study – activities of the
daily living (ADCS-ADLsev): p=0.003; severe impairment battery (SIB): p=0.002).
A pivotal monotherapy study of memantine in the treatment of mild to moderate Alzheimer’s disease
(MMSE total scores at baseline of 10 to 22) included 403 patients. Memantine-treated patients showed
a statistically significantly better effect than placebo-treated patients on the primary endpoints:
Alzheimer´s disease assessment scale (ADAS-cog) (p=0.003) and CIBIC-plus (p=0.004) at week 24
(last observation carried forward (LOCF)). In another monotherapy study in mild to moderate
Alzheimer’s disease a total of 470 patients (MMSE total scores at baseline of 11-23) were randomised.
In the prospectively defined primary analysis statistical significance was not reached at the primary
efficacy endpoint at week 24.
A meta-analysis of patients with moderate to severe Alzheimer’s disease (MMSE total scores < 20)
from the six phase III, placebo-controlled, 6-month studies (including monotherapy studies and studies
with patients on a stable dose of acetylcholinesterase inhibitors) showed that there was a statistically
significant effect in favour of memantine treatment for the cognitive, global, and functional domains.
When patients were identified with concurrent worsening in all three domains, results showed a
statistically significant effect of memantine in preventing worsening, as twice as many placebo-treated
patients as memantine-treated patients showed worsening in all three domains (21% vs. 11%,
p<0.0001).
5.2 Pharmacokineticproperties
Absorption:
Memantine has an absolute bioavailability of approximately 100%. t
max
is between 3 and
8 hours. There is no indication that food influences the absorption of memantine.
Distribution:
Daily doses of 20 mg lead to steady-state plasma concentrations of memantine ranging
from 70 to 150 ng/ml (0.5 - 1 µmol) with large interindividual variations. When daily doses of 5 to
30 mg were administered, a mean cerebrospinal fluid (CSF)/serum ratio of 0.52 was calculated. The
volume of distribution is around 10 l/kg. About 45% of memantine is bound to plasma-proteins.
Biotransformation:
In man, about 80% of the circulating memantine-related material is present as the
parent compound. Main human metabolites are N-3,5-dimethyl-gludantan, the isomeric mixture of 4-
and 6-hydroxy-memantine, and 1-nitroso-3,5-dimethyl-adamantane. None of these metabolites exhibit
NMDA-antagonistic activity. No cytochrome P 450 catalysed metabolism has been detected
in vitro.
In a study using orally administered
14
C-memantine, a mean of 84% of the dose was recovered within
20 days, more than 99% being excreted renally.
Elimination:
Memantine is eliminated in a monoexponential manner with a terminal t
½
of 60 to
100 hours. In volunteers with normal kidney function, total clearance (Cl
tot
) amounts to
170 ml/min/1.73 m² and part of total renal clearance is achieved by tubular secretion.
Renal handling also involves tubular reabsorption, probably mediated by cation transport proteins. The
renal elimination rate of memantine under alkaline urine conditions may be reduced by a factor of 7 to
9 (see section 4.4). Alkalisation of urine may result from drastic changes in diet, e.g. from a carnivore
to a vegetarian diet, or from the massive ingestion of alkalising gastric buffers.
Linearity:
Studies in volunteers have demonstrated linear pharmacokinetics in the dose range of 10 to
40 mg.
Pharmacokinetic/pharmacodynamic relationship:
At a dose of memantine of 20 mg per day the CSF
levels match the k
i
-value (k
i
= inhibition constant) of memantine, which is 0.5 µmol in human frontal
cortex.
5.3 Preclinical safety data
In short term studies in rats, memantine like other NMDA-antagonists have induced neuronal
vacuolisation and necrosis (Olney lesions) only after doses leading to very high peak serum
concentrations. Ataxia and other preclinical signs have preceded the vacuolisation and necrosis. As the
effects have neither been observed in long term studies in rodents nor in non-rodents, the clinical
relevance of these findings is unknown.
Ocular changes were inconsistently observed in repeat dose toxicity studies in rodents and dogs, but
not in monkeys. Specific ophthalmoscopic examinations in clinical studies with memantine did not
disclose any ocular changes.
Phospholipidosis in pulmonary macrophages due to accumulation of memantine in lysosomes was
observed in rodents. This effect is known from other active substances with cationic amphiphilic
properties. There is a possible relationship between this accumulation and the vacuolisation observed
in lungs. This effect was only observed at high doses in rodents. The clinical relevance of these
findings is unknown.
No genotoxicity has been observed following testing of memantine in standard assays. There was no
evidence of any carcinogenicity in life long studies in mice and rats. Memantine was not teratogenic in
rats and rabbits, even at maternally toxic doses, and no adverse effects of memantine were noted on
fertility. In rats, foetal growth reduction was noted at exposure levels, which are identical or slightly
higher than at human exposure.
6. PHARMACEUTICAL PARTICULARS
Potassium sorbate
Sorbitol E420
Purified water
4 years.
Once opened, the contents of the bottle should be used within 3 months.
6.4 Special precautions for storage
The bottle with the mounted pump may only be kept and transported in a vertical position.
6.5 Nature and contents of container
Brown glass bottles (Hydrolytic Class III) containing either 50, 100 g or 10 x 50 g solution.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
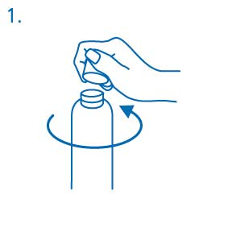
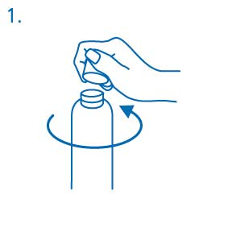
Prior to first use the dosing pump has to be screwed on the bottle. For removing the screw cap from
the bottle the cap must be turned anticlockwise and unscrewed completely (fig.1).
Mounting the dosing pump on the bottle:
The dosing pump has to be removed from the plastic bag (fig. 2) and placed on top of the bottle,
sliding the plastic dip tube carefully into the bottle. Then the dosing pump needs to be held onto the
neck of the bottle and screwed clockwise until it is firmly attached (fig 3). For the intended use the
dosing pump is only screwed on once when starting the use, and should never be unscrewed.
Use of the dosing pump for dispensing:
The dosing pump head has two positions and is easy to turn – anticlockwise (unlocked position) and
clockwise (locked position). The dosing pump head should not be pushed down while in the locked
position. The solution may only be dispensed in the unlocked position. To do this, the dosing pump
head has to be turned in the direction of the arrow about one eighth of a turn, until a resistance is felt
(fig. 4)
The dosing pump is then ready for use.
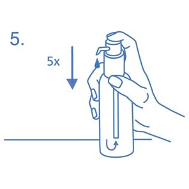
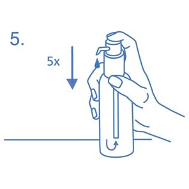
Preparing the dosing pump:
When used for the first time, the dosing pump does not dispense the correct amount of oral solution.
Therefore, the pump must be prepared (primed) by pushing the dosing pump head down completely
five times in succession (fig. 5).



The solution thus dispensed is discarded. The next time the dosing pump head is pushed downwards
completely, it dispenses the correct dose (1 dosing unit/stroke is equivalent to 0.5 ml oral solution, and
contains about 5 mg of the active substance memantine hydrochloride; fig. 6).
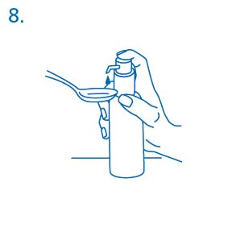
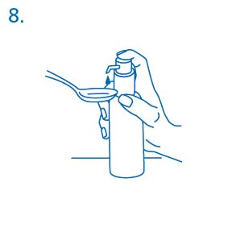
Correct use of the dosing pump:
The bottle should be placed on a flat, horizontal surface, for example a table top, and only use it in a
vertical position. A glass with a little water or a spoon should be hold below the nozzle and the dosing
pump head has to be pushed down in a firm but calm and steady manner (not too slowly) right down to
the stop (fig. 7, fig. 8).
The dosing pump head can then be released and is ready for the next downward stroke.
The dosing pump may only be used with the memantine hydrochloride solution in the bottle provided,
not for other substances or containers. If the pump does not function as described during intended use
and according to instruction, the patient should consult the treating physician or a pharmacist. The
dosing pump should be locked after use.


7. MARKETING AUTHORISATION HOLDER
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Denmark
8. MARKETING AUTHORISATION NUMBER(S)
EU/1/02/219/005-006
EU/1/02/219/013
9. DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 15/05/2002
Date of latest renewal: 15/05/2007
10. DATE OF REVISION OF THE TEXT
Detailed information on this product is available on the website of the European Medicines Agency
(EMA)
http://www.ema.europa.eu
1. NAME OF THE MEDICINAL PRODUCT
Ebixa 5 mg film-coated tablets.
Ebixa 10 mg film-coated tablets.
Ebixa 15 mg film-coated tablets.
Ebixa 20 mg film-coated tablets.
2. QUALITATIVE AND QUANTITATIVE COMPOSITION
Each film-coated tablet contains 5 mg of memantine hydrochloride equivalent to 4.15 mg memantine.
Each film-coated tablet contains 10 mg of memantine hydrochloride equivalent to 8.31 mg memantine.
Each film-coated tablet contains 15 mg of memantine hydrochloride equivalent to 12.46 mg memantine.
Each film-coated tablet contains 20 mg of memantine hydrochloride equivalent to 16.62 mg memantine.
For a full list of excipients, see section 6.1.
Film-coated tablets.
The 5 mg film-coated tablets are white to off-white, oval-oblong film-coated tablets with imprint ‘5’ on
one side and imprint ‘MEM’ on the other side.
The 10 mg film-coated tablets are pale yellow to yellow, oval shaped film-coated tablet with breaking
line and engravings “1 0” on one side and “M M” on the other side. The tablet can be divided into
equal halves.
The 15 mg film-coated tablets are orange to grey-orange, oval-oblong film-coated tablets with imprint
‘15’ on one side and imprint ‘MEM’ on the other side.
The 20 mg film-coated tablets are pale red to grey-red, oval-oblong film-coated tablets with imprint ‘20’
on one side and imprint ‘MEM’ on the other side.
4.1 Therapeuticindications
Treatment of patients with moderate to severe Alzheimer’s disease.
4.2 Posology and method of administration
Treatment should be initiated and supervised by a physician experienced in the diagnosis and
treatment of Alzheimer’s dementia. Therapy should only be started if a caregiver is available who will
regularly monitor the intake of the medicinal product by the patient. Diagnosis should be made
according to current guidelines.
Ebixa should be administered once a day and should be taken at the same time every day. The film-
coated tablets can be taken with or without food.
The recommended starting dose is 5 mg per day which is stepwise increased over the first 4 weeks of
treatment reaching the recommended maintenance dose as follows:
Week 1 (day 1-7):
The patient should take one 5 mg film-coated tablet per day (white to off-white, oval-oblong) for 7 days.
Week 2 (day 8-14):
The patient should take one 10 mg film-coated tablet per day (pale yellow to yellow, oval shaped) for 7
days.
Week 3 (day 15-21):
The patient should take one 15 mg film-coated tablet per day (grey-orange, oval-oblong) for 7 days.
Week 4 (day 22-28):
The patient should take one 20 mg film-coated tablet per day (grey-red, oval-oblong) for 7 days.
The maximum daily dose is 20 mg per day.
The recommended maintenance dose is 20 mg per day.
Elderly:
On the basis of the clinical studies, the recommended dose for patients over the age of 65
years is 20 mg per day (20 mg once a day) as described above.
Children and adolescents:
Ebixa is not recommended for use in children below 18 years due to a lack
of data on safety and efficacy.
Renal impairment:
In patients with mildly impaired renal function (creatinine clearance 50 – 80
ml/min) no dose adjustment is required. In patients with moderate renal impairment (creatinine
clearance 30 - 49 ml/min) daily dose should be 10 mg per day. If tolerated well after at least 7 days of
treatment, the dose could be increased up to 20 mg/day according to standard titration scheme. In
patients with severe renal impairment (creatinine clearance 5 – 29 ml/min) daily dose should be 10 mg
per day.
Hepatic impairment:
In patients with mild or moderate hepatic impaired function (Child-Pugh A and
Child-Pugh B), no dose adjustment is needed. No data on the use of memantine in patients with severe
hepatic impairment are available. Administration of Ebixa is not recommended in patients with severe
hepatic impairment.
Hypersensitivity to the active substance or to any of the excipients.
4.4 Special warnings and precautions for use
Caution is recommended in patients with epilepsy, former history of convulsions or patients with
predisposing factors for epilepsy.
Concomitant use of N-methyl-D-aspartate(NMDA)-antagonists such as amantadine, ketamine or
dextromethorphan should be avoided. These compounds act at the same receptor system as
memantine, and therefore adverse reactions (mainly central nervous system (CNS)-related) may be
more frequent or more pronounced (see also section 4.5).
Some factors that may raise urine pH (see section 5.2 “Elimination”) may necessitate careful
monitoring of the patient. These factors include drastic changes in diet, e.g. from a carnivore to a
vegetarian diet, or a massive ingestion of alkalising gastric buffers. Also, urine pH may be elevated by
states of renal tubulary acidosis (RTA) or severe infections of the urinary tract with
Proteus bacteria
.
In most clinical trials, patients with recent myocardial infarction, uncompensated congestive heart
failure (NYHA III-IV), or uncontrolled hypertension were excluded. As a consequence, only limited
data are available and patients with these conditions should be closely supervised.
4.5 Interaction with other medicinal products and other forms of interaction
Due to the pharmacological effects and the mechanism of action of memantine the following
interactions may occur:
The mode of action suggests that the effects of L-dopa, dopaminergic agonists, and
anticholinergics may be enhanced by concomitant treatment with NMDA-antagonists such as
memantine. The effects of barbiturates and neuroleptics may be reduced. Concomitant
administration of memantine with the antispasmodic agents, dantrolene or baclofen, can modify
their effects and a dose adjustment may be necessary.
Concomitant use of memantine and amantadine should be avoided, owing to the risk of
pharmacotoxic psychosis. Both compounds are chemically related NMDA-antagonists. The
same may be true for ketamine and dextromethorphan (see also section 4.4). There is one
published case report on a possible risk also for the combination of memantine and phenytoin.
Other active substances such as cimetidine, ranitidine, procainamide, quinidine, quinine and
nicotine that use the same renal cationic transport system as amantadine may also possibly
interact with memantine leading to a potential risk of increased plasma levels.
There may be a possibility of reduced serum level of hydrochlorothiazide (HCT) when
memantine is co-administered with HCT or any combination with HCT.
In post-marketing experience, isolated cases with international normalized ratio (INR) increases
have been reported in patients concomitantly treated with warfarin. Although no causal
relationship has been established, close monitoring of prothrombin time or INR is advisable for
patients concomitantly treated with oral anticoagulants.
In single-dose pharmacokinetic (PK) studies in young healthy subjects, no relevant active substance-
active substance interaction of memantine with glyburide/metformin or donepezil was observed.
In a clinical study in young healthy subjects, no relevant effect of memantine on the pharmacokinetics
of galantamine was observed.
Memantine did not inhibit CYP 1A2, 2A6, 2C9, 2D6, 2E1, 3A, flavin containing monooxygenase,
epoxide hydrolase or sulphation
in vitro
.
4.6 Pregnancy and lactation
For memantine, no clinical data on exposed pregnancies are available. Animal studies indicate a
potential for reducing intrauterine growth at exposure levels, which are identical or slightly higher
than at human exposure (see section 5.3). The potential risk for humans is unknown. Memantine
should not be used during pregnancy unless clearly necessary.
It is not known whether memantine is excreted in human breast milk but, taking into consideration the
lipophilicity of the substance, this probably occurs. Women taking memantine should not breast-feed.
4.7 Effects on ability to drive and use machines
Moderate to severe Alzheimer’s disease usually causes impairment of driving performance and
compromises the ability to use machinery. Furthermore, Ebixa has minor or moderate influence on the
ability to drive and use machines such that outpatients should be warned to take special care.
In clinical trials in mild to severe dementia, involving 1,784 patients treated with Ebixa and 1,595
patients treated with placebo, the overall incidence rate of adverse reactions with Ebixa did not differ
from those with placebo; the adverse reactions were usually mild to moderate in severity. The most
frequently occurring adverse reactions with a higher incidence in the Ebixa group than in the placebo
group were dizziness (6.3% vs 5.6%, respectively), headache (5.2% vs 3.9%), constipation (4.6% vs
2.6%), somnolence (3.4% vs 2.2%) and hypertension (4.1% vs 2.8%).
The following Adverse Reactions listed in the Table below have been accumulated in clinical studies
with Ebixa and since its introduction in the market. Within each frequency grouping, undesirable
effects are presented in order of decreasing seriousness.
Adverse reactions are ranked according to system organ class, using the following convention: very
common (≥1/10), common (≥1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥1/10,000 to <
1/1,000), very rare (< 1/10,000), not known (cannot be estimated from the available data).
Infections and infestations
Venous
thrombosis/thromboembolism
Respiratory, thoracic and mediastinal
disorders
Gastrointestinal disorders
General disorders and administration
site conditions
Uncommon Fatigue
1
Hallucinations have mainly been observed in patients with severe Alzheimer´s disease.
2
Isolated cases reported in post-marketing experience.
Alzheimer’s disease has been associated with depression, suicidal ideation and suicide. In post-
marketing experience these events have been reported in patients treated with Ebixa.









Only limited experience with overdose is available from clinical studies and post-marketing
experience.
Symptoms:
Relative large overdoses (200 mg and 105 mg/day for 3 days, respectively) have been
associated with either only symptoms of tiredness, weakness and/or diarrhoea or no symptoms. In the
overdose cases below 140 mg or unknown dose the patients revealed symptoms from central nervous
system (confusion, drowsiness, somnolence, vertigo, agitation, aggression, hallucination, and gait
disturbance) and/or of gastrointestinal origin (vomiting and diarrhoea).
In the most extreme case of overdose, the patient survived the oral intake of a total of 2000 mg
memantine with effects on the central nervous system (coma for 10 days, and later diplopia and
agitation). The patient received symptomatic treatment and plasmapheresis. The patient recovered
without permanent sequelae.
In another case of a large overdose, the patient also survived and recovered. The patient had received
400 mg memantine orally. The patient experienced central nervous system symptoms such as
restlessness, psychosis, visual hallucinations, proconvulsiveness, somnolence, stupor, and
unconsciousness.
Treatment:
In the event of overdose, treatment should be symptomatic. No specific antidote for
intoxication or overdose is available. Standard clinical procedures to remove active substance material,
e.g. gastric lavage, carbo medicinalis (interruption of potential entero-hepatic recirculation),
acidification of urine, forced diuresis should be used as appropriate.
In case of signs and symptoms of general central nervous system (CNS) overstimulation, careful
symptomatic clinical treatment should be considered.
5. PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamicproperties
Pharmacotherapeutic group: Other Anti-dementia drugs, ATC code: N06DX01.
There is increasing evidence that malfunctioning of glutamatergic neurotransmission, in particular at
NMDA-receptors, contributes to both expression of symptoms and disease progression in
neurodegenerative dementia.
Memantine is a voltage-dependent, moderate-affinity uncompetitive NMDA-receptor antagonist. It
modulates the effects of pathologically elevated tonic levels of glutamate that may lead to neuronal
dysfunction.
Clinical studies:
A pivotal monotherapy study in a population of patients suffering from moderate to
severe Alzheimer’s disease (mini mental state examination (MMSE) total scores at baseline of 3 - 14)
included a total of 252 outpatients. The study showed beneficial effects of memantine treatment in
comparison to placebo at 6 months (observed cases analysis for the clinician´s interview based
impression of change (CIBIC-plus): p=0.025; Alzheimer´s disease cooperative study – activities of
daily living (ADCS-ADLsev): p=0.003; severe impairment battery (SIB): p=0.002).
A pivotal monotherapy study of memantine in the treatment of mild to moderate Alzheimer’s disease
(MMSE total scores at baseline of 10 to 22) included 403 patients. Memantine-treated patients showed
a statistically significantly better effect than placebo-treated patients on the primary endpoints:
Alzheimer´s disease assessment scale (ADAS-cog) (p=0.003) and CIBIC-plus (p=0.004) at week 24
last observation carried forward (LOCF). In another monotherapy study in mild to moderate
Alzheimer’s disease a total of 470 patients (MMSE total scores at baseline of 11-23) were randomised.
In the prospectively defined primary analysis statistical significance was not reached at the primary
efficacy endpoint at week 24.
A meta-analysis of patients with moderate to severe Alzheimer’s disease (MMSE total scores < 20)
from the six phase III, placebo-controlled, 6-month studies (including monotherapy studies and studies
with patients on a stable dose of acetylcholinesterase inhibitors) showed that there was a statistically
significant effect in favour of memantine treatment for the cognitive, global, and functional domains.
When patients were identified with concurrent worsening in all three domains, results showed a
statistically significant effect of memantine in preventing worsening, as twice as many placebo-treated
patients as memantine-treated patients showed worsening in all three domains (21% vs. 11%,
p<0.0001).
5.2 Pharmacokineticproperties
Absorption:
Memantine has an absolute bioavailability of approximately 100%. t
max
is between 3 and
8 hours. There is no indication that food influences the absorption of memantine.
Distribution:
Daily doses of 20 mg lead to steady-state plasma concentrations of memantine ranging
from 70 to 150 ng/ml (0.5 - 1 µmol) with large interindividual variations. When daily doses of 5 to
30 mg were administered, a mean cerebrospinal fluid (CSF)/serum ratio of 0.52 was calculated. The
volume of distribution is around 10 l/kg. About 45% of memantine is bound to plasma-proteins.
Biotransformation:
In man, about 80% of the circulating memantine-related material is present as the
parent compound. Main human metabolites are N-3,5-dimethyl-gludantan, the isomeric mixture of 4-
and 6-hydroxy-memantine, and 1-nitroso-3,5-dimethyl-adamantane. None of these metabolites exhibit
NMDA-antagonistic activity. No cytochrome P 450 catalysed metabolism has been detected
in vitro.
In a study using orally administered
14
C-memantine, a mean of 84% of the dose was recovered within
20 days, more than 99% being excreted renally.
Elimination:
Memantine is eliminated in a monoexponential manner with a terminal t
½
of 60 to
100 hours. In volunteers with normal kidney function, total clearance (Cl
tot
) amounts to
170 ml/min/1.73 m² and part of total renal clearance is achieved by tubular secretion.
Renal handling also involves tubular reabsorption, probably mediated by cation transport proteins. The
renal elimination rate of memantine under alkaline urine conditions may be reduced by a factor of 7 to
9 (see section 4.4). Alkalisation of urine may result from drastic changes in diet, e.g. from a carnivore
to a vegetarian diet, or from the massive ingestion of alkalising gastric buffers.
Linearity:
Studies in volunteers have demonstrated linear pharmacokinetics in the dose range of 10 to
40 mg.
Pharmacokinetic/pharmacodynamic relationship:
At a dose of memantine of 20 mg per day the CSF
levels match the k
i
-value (k
i
= inhibition constant) of memantine, which is 0.5 µmol in human frontal
cortex.
5.3 Preclinical safety data
In short term studies in rats, memantine like other NMDA-antagonists have induced neuronal
vacuolisation and necrosis (Olney lesions) only after doses leading to very high peak serum
concentrations. Ataxia and other preclinical signs have preceded the vacuolisation and necrosis. As the
effects have neither been observed in long term studies in rodents nor in non-rodents, the clinical
relevance of these findings is unknown.
Ocular changes were inconsistently observed in repeat dose toxicity studies in rodents and dogs, but
not in monkeys. Specific ophthalmoscopic examinations in clinical studies with memantine did not
disclose any ocular changes.
Phospholipidosis in pulmonary macrophages due to accumulation of memantine in lysosomes was
observed in rodents. This effect is known from other active substances with cationic amphiphilic
properties. There is a possible relationship between this accumulation and the vacuolisation observed
in lungs. This effect was only observed at high doses in rodents. The clinical relevance of these
findings is unknown.
No genotoxicity has been observed following testing of memantine in standard assays. There was no
evidence of any carcinogenicity in life long studies in mice and rats. Memantine was not teratogenic in
rats and rabbits, even at maternally toxic doses, and no adverse effects of memantine were noted on
fertility. In rats, foetal growth reduction was noted at exposure levels, which are identical or slightly
higher than at human exposure.
6. PHARMACEUTICAL PARTICULARS
Tablet cores for 5/10/15/20 mg film-coated tablets:
Microcrystalline cellulose
Croscarmellose sodium
Colloidal anhydrous silica
Magnesium stearate
Tablet coat for 5/10/15/20 mg film-coated tablets:
Hypromellose
Macrogol 400
Titanium dioxide (E 171)
Additional for 10 mg film-coated tablets:
Iron oxide yellow (E 172)
Additional for 15 mg and 20 mg film-coated tablets:
Iron oxide yellow and red (E 172)
6.4 Special precautions for storage
This medicinal product does not require any special storage conditions.
6.5 Nature and contents of container
Each pack contains 28 film-coated tablets in 4 PVDC/PE/PVC/Al-blister or PP/Al-blisters with 7 film-
coated tablets of 5 mg, 7 film-coated tablets of 10 mg, 7 film-coated tablets of 15 mg and 7 film-
coated tablets of 20 mg.
6.6 Special precautions for disposal
7. MARKETING AUTHORISATION HOLDER
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Denmark
8. MARKETING AUTHORISATION NUMBER(S)
EU/1/02/219/022
EU/1/02/219/036
9. DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 08/05/2008
Date of latest renewal:
10. DATE OF REVISION OF THE TEXT
Detailed information on this product is available on the website of the European Medicines Agency
(EMA) http://www.ema.europa.eu
The active substance is memantine hydrochloride. Each film-coated tablet contains 20 mg memantine
hydrochloride equivalent to 16.62 mg memantine.
The other ingredients are microcrystalline cellulose, croscarmellose sodium, colloidal anhydrous
silica, magnesium stearate, all in the tablet core; and hypromellose, macrogol 400, titanium dioxide (E
171), iron oxide yellow and red (E 172), all in the tablet coating.
What Ebixa looks like and contents of the pack
Ebixa film-coated tablets are presented as pale red to grey-red, oval-oblong film-coated tablets with
imprint ‘20’ on one side and imprint ‘MEM’ on the other side.
Ebixa film-coated tablets are available in blister packs of 14 tablets, 28 tablets, 42 tablets, 49 x 1
tablets,
56 tablets, 56 x 1 tablets, 70 tablets, 84 tablets, 98 tablets, 98 x 1 tablets, 100 x 1 tablets, 112
tablets or 840 (20 x 42) tablets. The pack sizes 49 x 1, 56 x 1, 98 x 1 and 100 x 1 film-coated tablets
are presented in unit dose blister
.
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Denmark.
For any information about this medicine, please contact the local representative of the Marketing
Authorisation Holder.
Belgique/België/Belgien
Lundbeck S.A./N.V.
Avenue Molière 225
B-1050 Bruxelles/Brussel/Brüssel
Tél/Tel: +32 2 340 2828
Luxembourg/Luxemburg
Lundbeck S.A.
Avenue Molière 225
B-1050 Bruxelles/Brussel
Tél: +32 2 340 2828
България
Lundbeck Export A/S Representative Office
EXPO 2000
Vaptzarov Blvd. 55
Sofia 1407
Tel: +359 2 962 4696
Magyarország
Lundbeck Hungaria Kft.
Montevideo utca 3/B
H-1037 Budapest
Tel: +36 1 4369980
Česká republika
Lundbeck Česká republika s.r.o.
Bozděchova 7
CZ-150 00 Praha 5
Tel: +420 225 275 600
Malta
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Denmark
Tel: + 45 36301311
Danmark
Lundbeck Pharma A/S
Dalbergstrøget 5
DK-2630 Taastrup
Tlf: +45 4371 4270
Nederland
Lundbeck B.V.
Herikerbergweg 100
NL-1101 CM Amsterdam
Tel: +31 20 697 1901
Deutschland
Lundbeck GmbH
Karnapp 25
D-21079 Hamburg
Tel: +49 40 23649 0
Norge
H. Lundbeck AS
Postboks 361
N-1326 Lysaker
Tlf: +47 91 300 800
Eesti
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Taani
Tel: + 45 36301311
Österreich
Lundbeck Austria GmbH
Dresdner Straße 82
A-1200 Wien
Tel: +43 1 331 070
Ελλάδα
Lundbeck Hellas S.A.
Λεωφόρος Κηφισίας 64
GR-151 25 Μαρούσι, Αθήνα
Τηλ: +30 210 610 5036
Polska
Lundbeck Poland Sp. z o. o.
ul. Krzywickiego 34
PL-02-078 Warszawa
Tel.: + 48 22 626 93 00
España
Lundbeck España S.A.
Av. Diagonal, 605, 9-1a
E-08028 Barcelona
Tel: +34 93 494 9620
Portugal
Lundbeck Portugal Lda
Quinta da Fonte
Edifício D. João I – Piso 0 Ala A
P-2770-203 Paço d’Arcos
Tel: +351 21 00 45 900
France
Lundbeck SAS
37-45, quai du Président Roosevelt
F-92445 Issy-les-Moulineaux Cedex
Tél: + 33 1 79 41 29 00
România
Lundbeck Export A/S
Reprezentanta din Romania
Str. Ghiocei no.7A, sector 2
Bucureşti, 020571 - RO
Tel: +40 21319 88 26
Ireland
Lundbeck (Ireland) Limited
7 Riverwalk
Citywest Business Campus
IRL-Dublin 24
Tel: +353 1 468 9800
Slovenija
Lundbeck Pharma d.o.o.
Titova cesta 8
SI-2000 Maribor
Tel.: +386 2 229 4500
Ísland
Lundbeck Export A/S, útibú á Íslandi
Ármúla 1
IS-108 Reykjavík
Tel: +354 414 7070
Slovenská republika
Lundbeck Slovensko s.r.o.
Zvolenská 19
SK-821 09 Bratislava 2
Tel: +421 2 5341 42 18
Italia
Lundbeck Italia S.p.A.
Via G. Fara 35
I-20124 Milan
Tel: +39 02 677 4171
Suomi/Finland
Oy H. Lundbeck Ab
Itäinen Pitkäkatu 4/Österlånggatan 4
FI-20520 Turku/Åbo
Puh/Tel: +358 2 276 5000
Κύπρος
Lundbeck Hellas A.E
Θεμ. Δέρβη-Φλωρίνης
STADYL BUILDING
CY-1066 Λευκωσία
Τηλ.: +357 22490305
Sverige
H. Lundbeck AB
Rundgången 30 B
Box 23
S-250 53 Helsingborg
Tel: +46 4225 4300
Latvija
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Dānija
Tel: + 45 36301311
United Kingdom
Lundbeck Limited
Lundbeck House
Caldecotte Lake Business Park
Caldecotte
Milton Keynes MK7 8LG - UK
Tel: +44 1908 64 9966
Lietuva
H. Lundbeck A/S
Ottiliavej 9
DK-2500 Valby
Danija
Tel: + 45 36301311
This leaflet was last approved in MM/YYYY
Detailed information on this product is available on the website of the European Medicines Agency
(EMA) http://www.ema.europa.eu
Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/ebixa.html
Copyright © 1995-2021 ITA all rights reserved.
|

































 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































