Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
GONAL-f 75 IU (5.5 micrograms) powder and solvent for solution for injection.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each vial contains 5.5 micrograms of follitropin alfa* equivalent to 75 IU. Each ml of the
reconstituted solution contains 75 IU.
* recombinant human follicle stimulating hormone (r-hFSH) produced in Chinese Hamster Ovary
(CHO) cells by recombinant DNA technology.
For a full list of excipients, see section 6.1.
Powder and solvent for solution for injection.
Appearance of the powder: white lyophilised pellet.
Appearance of the solvent: clear colourless solution.
The pH of the reconstituted solution is 6.5-7.5.
4.1 Therapeutic indications
• Anovulation (including polycystic ovarian syndrome) in women who have been unresponsive to
treatment with clomiphene citrate.
• Stimulation of multifollicular development in women undergoing superovulation for assisted
reproductive technologies (ART) such as
in vitro
fertilisation (IVF), gamete intra-fallopian
transfer and zygote intra-fallopian transfer.
• GONAL-f in association with a luteinising hormone (LH) preparation is recommended for the
stimulation of follicular development in women with severe LH and FSH deficiency. In clinical
trials these patients were defined by an endogenous serum LH level < 1.2 IU/l.
• GONAL-f is indicated for the stimulation of spermatogenesis in men who have congenital or
acquired hypogonadotrophic hypogonadism with concomitant human Chorionic Gonadotropin
(hCG) therapy.
4.2 Posology and method of administration
Treatment with GONAL-f should be initiated under the supervision of a physician experienced in the
treatment of fertility disorders.
The dose recommendations given for GONAL-f are those in use for urinary FSH. Clinical assessment
of GONAL-f indicates that its daily doses, regimens of administration, and treatment monitoring
procedures should not be different from those currently used for urinary FSH-containing medicinal
products. It is advised to adhere to the recommended starting doses indicated below.
Comparative clinical studies have shown that on average patients require a lower cumulative dose and
shorter treatment duration with GONAL-f compared with urinary FSH. Therefore, it is considered
appropriate to give a lower total dose of GONAL-f than generally used for urinary FSH, not only in
order to optimise follicular development but also to minimise the risk of unwanted ovarian
hyperstimulation. See section 5.1.
Women with anovulation (including polycystic ovarian syndrome)
GONAL-f may be given as a course of daily injections. In menstruating women treatment should
commence within the first 7 days of the menstrual cycle.
A commonly used regimen commences at 75-150 IU FSH daily and is increased preferably by 37.5 or
75 IU at 7 or preferably 14 day intervals if necessary, to obtain an adequate, but not excessive,
response. Treatment should be tailored to the individual patient’s response as assessed by measuring
follicle size by ultrasound and/or oestrogen secretion. The maximal daily dose is usually not higher
than 225 IU FSH. If a patient fails to respond adequately after 4 weeks of treatment, that cycle should
be abandoned and the patient should undergo further evaluation after which she may recommence
treatment at a higher starting dose than in the abandoned cycle.
When an optimal response is obtained, a single injection of 250 micrograms recombinant human
choriogonadotropin alfa (r-hCG) or 5,000 IU, up to 10,000 IU hCG should be administered
24-48 hours after the last GONAL-f injection. The patient is recommended to have coitus on the day
of, and the day following, hCG administration. Alternatively intrauterine insemination (IUI) may be
performed.
If an excessive response is obtained, treatment should be stopped and hCG withheld (see section 4.4).
Treatment should recommence in the next cycle at a dose lower than that of the previous cycle.
Women undergoing ovarian stimulation for multiple follicular development prior to in vitro
fertilisation or other assisted reproductive technologies.
A commonly used regimen for superovulation involves the administration of 150-225 IU of GONAL-f
daily, commencing on days 2 or 3 of the cycle. Treatment is continued until adequate follicular
development has been achieved (as assessed by monitoring of serum oestrogen concentrations and/or
ultrasound examination), with the dose adjusted according to the patient’s response, to usually not
higher than 450 IU daily. In general adequate follicular development is achieved on average by the
tenth day of treatment (range 5 to 20 days).
A single injection of 250 micrograms r-hCG or 5,000 IU up to 10,000 IU hCG is administered
24-48 hours after the last GONAL-f injection to induce final follicular maturation.
Down-regulation with a gonadotropin-releasing hormone (GnRH) agonist or antagonist is now
commonly used in order to suppress the endogenous LH surge and to control tonic levels of LH. In a
commonly used protocol, GONAL-f is started approximately 2 weeks after the start of agonist
treatment, both being continued until adequate follicular development is achieved. For example,
following two weeks of treatment with an agonist, 150-225 IU GONAL-f are administered for the first
7 days. The dose is then adjusted according to the ovarian response.
Overall experience with IVF indicates that in general the treatment success rate remains stable during
the first four attempts and gradually declines thereafter.
Women with anovulation resulting from severe LH and FSH deficiency.
In LH and FSH deficient women (hypogonadotrophic hypogonadism), the objective of GONAL-f
therapy in association with lutropin alfa is to develop a single mature Graafian follicle from which the
oocyte will be liberated after the administration of human chorionic gonadotropin (hCG). GONAL-f
should be given as a course of daily injections simultaneously with lutropin alfa. Since these patients
are amenorrhoeic and have low endogenous oestrogen secretion, treatment can commence at any time.
A recommended regimen commences at 75 IU of lutropin alfa daily with 75-150 IU FSH. Treatment
should be tailored to the individual patient’s response as assessed by measuring follicle size by
ultrasound and oestrogen response.
If an FSH dose increase is deemed appropriate, dose adaptation should preferably be after 7-14 day
intervals and preferably by 37.5-75 IU increments. It may be acceptable to extend the duration of
stimulation in any one cycle to up to 5 weeks.
When an optimal response is obtained, a single injection of 250 micrograms r-hCG or 5,000 IU up to
10,000 IU hCG should be administered 24-48 hours after the last GONAL-f and lutropin alfa
injections. The patient is recommended to have coitus on the day of, and on the day following, hCG
administration.
Alternatively, IUI may be performed.
Luteal phase support may be considered since lack of substances with luteotrophic activity (LH/hCG)
after ovulation may lead to premature failure of the corpus luteum.
If an excessive response is obtained, treatment should be stopped and hCG withheld. Treatment should
recommence in the next cycle at a dose of FSH lower than that of the previous cycle.
Men with hypogonadotrophic hypogonadism
GONAL-f should be given at a dose of 150 IU three times a week, concomitantly with hCG, for a
minimum of 4 months. If after this period, the patient has not responded, the combination treatment
may be continued; current clinical experience indicates that treatment for at least 18 months may be
necessary to achieve spermatogenesis.
There is no relevant use of GONAL-f in the elderly population. Safety and effectiveness of GONAL-f
in elderly patients have not been established.
Renal or hepatic impairment
Safety, efficacy and pharmacokinetics of GONAL-f in patients with renal or hepatic impairment have
not been established.
There is no relevant use of GONAL-f in the paediatric population.
GONAL-f is intended for subcutaneous administration. The first injection of GONAL--f should be
performed under direct medical supervision. Self-administration of GONAL-f should only be
performed by patients who are well motivated, adequately trained and have access to expert advice.
The injection site should be alternated daily.
For instructions on the reconstitution and administration of GONAL-f powder and solvent for solution
for injection see section 6.6 and the package leaflet.
• hypersensitivity to the active substance follitropin alfa, FSH or to any of the excipients
• tumours of the hypothalamus or pituitary gland
• ovarian enlargement or ovarian cyst not due to polycystic ovarian syndrome
• gynaecological haemorrhages of unknown aetiology
• ovarian, uterine or mammary carcinoma
GONAL-f must not be used when an effective response cannot be obtained, such as:
• primary ovarian failure
• malformations of sexual organs incompatible with pregnancy
• fibroid tumours of the uterus incompatible with pregnancy
• primary testicular insufficiency
4.4 Special warnings and precautions for use
GONAL-f is a potent gonadotrophic substance capable of causing mild to severe adverse reactions,
and should only be used by physicians who are thoroughly familiar with infertility problems and their
management.
Gonadotropin therapy requires a certain time commitment by physicians and supportive health
professionals, as well as the availability of appropriate monitoring facilities. In women, safe and
effective use of GONAL-f calls for monitoring of ovarian response with ultrasound, alone or
preferably in combination with measurement of serum oestradiol levels, on a regular basis. There may
be a degree of interpatient variability in response to FSH administration, with a poor response to FSH
in some patients and exaggerated response in others. The lowest effective dose in relation to the
treatment objective should be used in both men and women.
Patients with porphyria or a family history of porphyria should be closely monitored during treatment
with GONAL-f. Deterioration or a first appearance of this condition may require cessation of
treatment.
Before starting treatment, the couple’s infertility should be assessed as appropriate and putative
contraindications for pregnancy evaluated. In particular, patients should be evaluated for
hypothyroidism, adrenocortical deficiency, hyperprolactinemia and appropriate specific treatment
given.
Patients undergoing stimulation of follicular growth, whether as treatment for anovulatory infertility or
ART procedures, may experience ovarian enlargement or develop hyperstimulation. Adherence to
recommended GONAL-f dose and regimen of administration and careful monitoring of therapy will
minimise the incidence of such events. For accurate interpretation of the indices of follicle
development and maturation, the physician should be experienced in the interpretation of the relevant
tests.
In clinical trials, an increase of the ovarian sensitivity to GONAL-f was shown when administered
with lutropin alfa. If an FSH dose increase is deemed appropriate, dose adaptation should preferably
be at 7-14 day intervals and preferably with 37.5-75 IU increments.
No direct comparison of GONAL-f/LH versus human menopausal gonadotropin (hMG) has been
performed. Comparison with historical data suggests that the ovulation rate obtained with
GONAL-f/LH is similar to that obtained with hMG.
Ovarian Hyperstimulation Syndrome (OHSS)
A certain degree of ovarian enlargement is an expected effect of controlled ovarian stimulation. It is
more commonly seen in women with polycystic ovarian syndrome and usually regresses without
treatment.
In distinction to uncomplicated ovarian enlargement, OHSS is a condition that can manifest itself with
increasing degrees of severity. It comprises marked ovarian enlargement, high serum sex steroids, and
an increase in vascular permeability which can result in an accumulation of fluid in the peritoneal,
pleural and, rarely, in the pericardial cavities.
The following symptomatology may be observed in severe cases of OHSS: abdominal pain, abdominal
distension, severe ovarian enlargement, weight gain, dyspnoea, oliguria and gastrointestinal symptoms
including nausea, vomiting and diarrhoea. Clinical evaluation may reveal hypovolaemia,
haemoconcentration, electrolyte imbalances, ascites, haemoperitoneum, pleural effusions,
hydrothorax, or acute pulmonary distress. Very rarely, severe OHSS may be complicated by ovarian
torsion or thromboembolic events such as pulmonary embolism, ischaemic stroke or myocardial
infarction.
Independent risk factors for developing OHSS include polycystic ovarian syndrome high absolute or
rapidly rising serum oestradiol levels (e.g. > 900 pg/ml or > 3,300 pmol/l in anovulation;
> 3,000 pg/ml or > 11,000 pmol/l in ART) and large number of developing ovarian follicles (e.g.
> 3 follicles of ≥ 14 mm in diameter in anovulation; ≥ 20 follicles of ≥ 12 mm in diameter in ART).
Adherence to recommended GONAL-f dose and regimen of administration can minimise the risk of
ovarian hyperstimulation (see sections 4.2 and 4.8). Monitoring of stimulation cycles by ultrasound
scans as well as oestradiol measurements are recommended to early identify risk factors.
There is evidence to suggest that hCG plays a key role in triggering OHSS and that the syndrome may
be more severe and more protracted if pregnancy occurs. Therefore, if signs of ovarian
hyperstimulation occur such as serum oestradiol level > 5,500 pg/ml or > 20,200 pmol/l and/or ≥ 40
follicles in total, it is recommended that hCG be withheld and the patient be advised to refrain from
coitus or to use barrier contraceptive methods for at least 4 days. OHSS may progress rapidly (within
24 hours) or over several days to become a serious medical event. It most often occurs after hormonal
treatment has been discontinued and reaches its maximum at about seven to ten days following
treatment. Therefore patients should be followed for at least two weeks after hCG administration.
In ART, aspiration of all follicles prior to ovulation may reduce the occurrence of hyperstimulation.
Mild or moderate OHSS usually resolves spontaneously. If severe OHSS occurs, it is recommended
that gonadotropin treatment be stopped if still ongoing, and that the patient be hospitalised and
appropriate therapy be started.
In patients undergoing ovulation induction, the incidence of multiple pregnancy is increased compared
with natural conception. The majority of multiple conceptions are twins. Multiple pregnancy,
especially of high order, carries an increased risk of adverse maternal and perinatal outcomes.
To minimise the risk of multiple pregnancy, careful monitoring of ovarian response is recommended.
In patients undergoing ART procedures the risk of multiple pregnancy is related mainly to the number
of embryos replaced, their quality and the patient age.
The patients should be advised of the potential risk of multiple births before starting treatment.
The incidence of pregnancy loss by miscarriage or abortion is higher in patients undergoing
stimulation of follicular growth for ovulation induction or ART than following natural conception.
Women with a history of tubal disease are at risk of ectopic pregnancy, whether the pregnancy is
obtained by spontaneous conception or with fertility treatments. The prevalence of ectopic pregnancy
after ART, was reported to be higher than in the general population.
Reproductive system neoplasms
There have been reports of ovarian and other reproductive system neoplasms, both benign and
malignant, in women who have undergone multiple treatment regimens for infertility treatment. It is
not yet established whether or not treatment with gonadotropins increases the risk of these tumours in
infertile women.
The prevalence of congenital malformations after ART may be slightly higher than after spontaneous
conceptions. This is thought to be due to differences in parental characteristics (e.g. maternal age,
sperm characteristics) and multiple pregnancies.
In women with recent or ongoing thromboembolic disease or women with generally recognised risk
factors for thrombo-embolic events, such as personal or family history, treatment with gonadotropins
may further increase the risk for aggravation or occurrence of such events. In these women, the
benefits of gonadotropin administration need to be weighed against the risks. It should be noted
however that pregnancy itself as well as OHSS also carry an increased risk of thrombo-embolic
events.
Elevated endogenous FSH levels are indicative of primary testicular failure. Such patients are
unresponsive to GONAL-f/hCG therapy. GONAL-f should not be used when an effective response
cannot be obtained.
Semen analysis is recommended 4 to 6 months after the beginning of treatment as part of the
assessment of the response.
GONAL-f contains less than 1 mmol sodium (23 mg) per dose, i.e. essentially “sodium-free”.
4.5 Interaction with other medicinal products and other forms of interaction
Concomitant use of GONAL-f with other medicinal products used to stimulate ovulation (e.g. hCG,
clomiphene citrate) may potentiate the follicular response, whereas concurrent use of a GnRH agonist
or antagonist to induce pituitary desensitisation may increase the dose of GONAL-f needed to elicit an
adequate ovarian response. No other clinically significant medicinal product interaction has been
reported during GONAL-f therapy.
4.6 Fertility, pregnancy and lactation
Pregnancy
There is no indication for use of GONAL-f during pregnancy. Data on a limited number of exposed
pregnancies (less than 300 pregnancy outcomes) indicate no malformative or feto/neonatal toxicity of
follitropin alfa.
No teratogenic effect has been observed in animal studies (see section 5.3).
In case of exposure during pregnancy, clinical data are not sufficient to exclude a teratogenic effect of
GONAL-f.
Breastfeeding
GONAL-f is not indicated during breastfeeding.
Fertility
GONAL-f is indicated for use in infertility (see section 4.1).
4.7 Effects on ability to drive and use machines
GONAL-f is expected to have no or negligible influence on the ability to drive and use machines.
The most commonly reported adverse reactions are headache, ovarian cysts and local injection site
reactions (e.g. pain, erythema, haematoma, swelling and/or irritation at the site of injection).
Mild or moderate ovarian hyperstimulation syndrome (OHSS) have been commonly reported and
should be considered as an intrinsic risk of the stimulation procedure. Severe OHSS is uncommon (see
section 4.4).
Thromboembolism may occur very rarely, usually associated with severe OHSS (see section 4.4).
The following definitions apply to the frequency terminology used hereafter:
Very common (≥ 1/10)
Common (≥ 1/100 to < 1/10)
Uncommon (≥ 1/1,000 to < 1/100)
Rare (≥ 1/10,000 to < 1/1,000)
Very rare (< 1/10,000)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Nervous system disorders
Very common: Headache
Vascular disorders
Very rare: Thromboembolism, usually associated with severe OHSS (see section 4.4)
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Gastrointestinal disorders
Common: Abdominal pain, abdominal distension, abdominal discomfort, nausea, vomiting,
diarrhoea
Reproductive system and breast disorders
Very common: Ovarian cysts
Common:
Mild or moderate OHSS (including associated symptomatology)
Severe OHSS (including associated symptomatology) (see section 4.4)
Complication of severe OHSS
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Skin and subcutaneous tissue disorders
Common: Acne
Reproductive system and breast disorders
Common: Gynaecomastia,Varicocele
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Investigations
Common: Weightgain
The effects of an overdose of GONAL-f are unknown, nevertheless, there is a possibility that OHSS
may occur (see section 4.4).
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: Sex hormones and modulators of the genital systems, gonadotropins,
ATC code: G03GA05.
In women, the most important effect resulting from parenteral administration of FSH is the
development of mature Graafian follicles.
In women with anovulation, the object of GONAL-f therapy
is to develop a single mature Graafian follicle from which the ovum will be liberated after the
administration of hCG.
Clinical efficacy and safety in women
In clinical trials, patients with severe FSH and LH deficiency were defined by an endogenous serum
LH level < 1.2 IU/l as measured in a central laboratory. However, it should be taken into account that
there are variations between LH measurements performed in different laboratories.
In clinical studies comparing r-hFSH (follitropin alfa) and urinary FSH in ART (see table below) and
in ovulation induction, GONAL-f was more potent than urinary FSH in terms of a lower total dose and
a shorter treatment period needed to trigger follicular maturation.
In ART, GONAL-f at a lower total dose and shorter treatment period than urinary FSH, resulted in a
higher number of oocytes retrieved when compared to urinary FSH.
Table: Results of study GF 8407 (randomised parallel group study comparing efficacy and safety of
GONAL-f with urinary FSH in assisted reproduction technologies)
Number of oocytes retrieved
Days of FSH stimulation required
Total dose of FSH required (number
of FSH 75 IU ampoules)
Need to increase the dose (%) 56.2 85.3
Differences between the 2 groups were statistically significant (p< 0.05) for all criteria listed.
Clinical efficacy and safety in men
In men deficient in FSH, GONAL-f administered concomitantly with hCG for at least 4 months
induces spermatogenesis.
5.2 Pharmacokinetic properties
Following intravenous administration, follitropin alfa is distributed to the extracellular fluid space with
an initial half-life of around 2 hours and eliminated from the body with a terminal half-life of about
one day. The steady state volume of distribution and total clearance are 10 l and 0.6 l/h, respectively.
One-eighth of the follitropin alfa dose is excreted in the urine.
Following subcutaneous administration, the absolute bioavailability is about 70 %. Following repeated
administration, follitropin alfa accumulates 3-fold achieving a steady-state within 3-4 days. In women
whose endogenous gonadotropin secretion is suppressed, follitropin alfa has nevertheless been shown
to effectively stimulate follicular development and steroidogenesis, despite unmeasurable LH levels.
5.3 Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of single and
repeated dose toxicity and genotoxicity additional to that already stated in other sections of this SmPC.
Impaired fertility has been reported in rats exposed to pharmacological doses of follitropin alfa
(≥ 40 IU/kg/day) for extended periods, through reduced fecundity.
Given in high doses (≥ 5 IU/kg/day) follitropin alfa caused a decrease in the number of viable foetuses
without being a teratogen, and dystocia similar to that observed with urinary Menopausal
Gonadotropin (hMG). However, since GONAL-f is not indicated in pregnancy, these data are of
limited clinical relevance.









PHARMACEUTICAL PARTICULARS
Sucrose
Sodium dihydrogen phosphate monohydrate
Disodium phosphate dihydrate
Methionine
Polysorbate 20
Phosphoric acid, concentrated
Sodium hydroxide
This medicinal product must not be mixed with other medicinal products except those mentioned in
section 6.6.
For immediate and single use following first opening and reconstitution.
6.4 Special precautions for storage
Store in the original package, in order to protect from light.
6.5 Nature and contents of container
GONAL f is presented as a powder and solvent for injection. The powder is presented in 3 ml vials
(Type I glass), with rubber stopper (bromobutyl rubber) and aluminium flip-off cap. The 1 ml solvent
for reconstitution is presented in either 2 or 3 ml vials (Type I glass) with rubber stopper
(teflon-coated rubber) or in 1 ml pre-filled syringes (Type I glass) with a rubber stopper.
The medicinal product is supplied in packs of 1 vial with 1 vial of solvent, or packs of 1, 5, or 10 vials
with 1, 5 or 10 of solvent pre-filled syringe.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
GONAL-f must be reconstituted with the solvent before use (see section “How to prepare and use the
GONAL-f powder and solvent” in the package leaflet).
GONAL-f may be co-reconstituted with lutropin alfa and co-administered as a single injection. In this
case lutropin alfa should be reconstituted first and then used to reconstitute GONAL-f powder.
Studies have shown that co-administration with lutropin alfa, does not significantly alter the activity,
stability, pharmacokinetic nor pharmacodynamic properties of the active substances.
The reconstituted solution should not be administered if it contains particles or is not clear.
Any unused medicinal product or waste material should be disposed of in accordance with local
requirements.
MARKETING AUTHORISATION HOLDER
Merck Serono Europe Ltd.
56 Marsh Wall
London E14 9TP
United Kingdom
MARKETING AUTHORISATION NUMBERS
EU/1/95/001/005
EU/1/95/001/025
EU/1/95/001/026
EU/1/95/001/027
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 20 October 1995.
Date of last renewal: 20 October 2005.
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency http://www.ema.europa.eu
NAME OF THE MEDICINAL PRODUCT
GONAL-f 1050 IU/1.75 ml (77 micrograms/1.75 ml) powder and solvent for solution for injection.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each vial contains 77 micrograms of follitropin alfa* equivalent to 1050 IU. Each ml of the
reconstituted solution contains 600 IU.
* recombinant human follicle stimulating hormone (r-hFSH) produced in Chinese Hamster Ovary
(CHO) cells by recombinant DNA technology.
For a full list of excipients, see section 6.1.
Powder and solvent for solution for injection.
Appearance of the powder: white lyophilised pellet.
Appearance of the solvent: clear colourless solution.
The pH of the reconstituted solution is 6.5-7.5.
4.1 Therapeutic indications
• Anovulation (including polycystic ovarian syndrome) in women who have been unresponsive to
treatment with clomiphene citrate.
• Stimulation of multifollicular development in women undergoing superovulation for assisted
reproductive technologies (ART) such as
in vitro
fertilisation (IVF), gamete intra-fallopian
transfer and zygote intra-fallopian transfer.
• GONAL-f in association with a luteinising hormone (LH) preparation is recommended for the
stimulation of follicular development in women with severe LH and FSH deficiency. In clinical
trials these patients were defined by an endogenous serum LH level < 1.2 IU/l.
• GONAL-f is indicated for the stimulation of spermatogenesis in men who have congenital or
acquired hypogonadotrophic hypogonadism with concomitant human Chorionic Gonadotropin
(hCG) therapy.
4.2 Posology and method of administration
Treatment with GONAL-f should be initiated under the supervision of a physician experienced in the
treatment of fertility disorders.
The dose recommendations given for GONAL-f are those in use for urinary FSH. Clinical assessment
of GONAL-f indicates that its daily doses, regimens of administration, and treatment monitoring
procedures should not be different from those currently used for urinary FSH-containing medicinal
products. It is advised to adhere to the recommended starting doses indicated below.
Comparative clinical studies have shown that on average patients require a lower cumulative dose and
shorter treatment duration with GONAL-f compared with urinary FSH. Therefore, it is considered
appropriate to give a lower total dose of GONAL-f than generally used for urinary FSH, not only in
order to optimise follicular development but also to minimise the risk of unwanted ovarian
hyperstimulation. See section 5.1.
Bioequivalence has been demonstrated between equivalent doses of the monodose presentation and
the multidose presentation of GONAL-f.
The following table states the volume to be administered to deliver the prescribed dose:
Volume to be injected (ml)
The next injection should be done at the same time the next day.
Women with anovulation (including polycystic ovarian syndrome)
GONAL-f may be given as a course of daily injections. In menstruating women treatment should
commence within the first 7 days of the menstrual cycle.
A commonly used regimen commences at 75-150 IU FSH daily and is increased preferably by 37.5 or
75 IU at 7 or preferably 14 day intervals if necessary, to obtain an adequate, but not excessive,
response. Treatment should be tailored to the individual patient’s response as assessed by measuring
follicle size by ultrasound and/or oestrogen secretion. The maximal daily dose is usually not higher
than 225 IU FSH. If a patient fails to respond adequately after 4 weeks of treatment, that cycle should
be abandoned and the patient should undergo further evaluation after which she may recommence
treatment at a higher starting dose than in the abandoned cycle.
When an optimal response is obtained, a single injection of 250 micrograms recombinant human
choriogonadotropin alfa (r-hCG) or 5,000 IU, up to 10,000 IU hCG should be administered
24-48 hours after the last GONAL-f injection. The patient is recommended to have coitus on the day
of, and the day following, hCG administration. Alternatively intrauterine insemination (IUI) may be
performed.
If an excessive response is obtained, treatment should be stopped and hCG withheld (see section 4.4).
Treatment should recommence in the next cycle at a dose lower than that of the previous cycle.
Women undergoing ovarian stimulation for multiple follicular development prior to in vitro
fertilisation or other assisted reproductive technologies.
A commonly used regimen for superovulation involves the administration of 150-225 IU of GONAL-f
daily, commencing on days 2 or 3 of the cycle. Treatment is continued until adequate follicular
development has been achieved (as assessed by monitoring of serum oestrogen concentrations and/or
ultrasound examination), with the dose adjusted according to the patient’s response, to usually not









higher than 450 IU daily. In general adequate follicular development is achieved on average by the
tenth day of treatment (range 5 to 20 days).
A single injection of 250 micrograms r-hCG or 5,000 IU up to 10,000 IU hCG is administered
24-48 hours after the last GONAL-f injection to induce final follicular maturation.
Down-regulation with a gonadotropin-releasing hormone (GnRH) agonist or antagonist is now
commonly used in order to suppress the endogenous LH surge and to control tonic levels of LH. In a
commonly used protocol, GONAL-f is started approximately 2 weeks after the start of agonist
treatment, both being continued until adequate follicular development is achieved. For example,
following two weeks of treatment with an agonist, 150-225 IU GONAL-f are administered for the first
7 days. The dose is then adjusted according to the ovarian response.
Overall experience with IVF indicates that in general the treatment success rate remains stable during
the first four attempts and gradually declines thereafter.
Women with anovulation resulting from severe LH and FSH deficiency.
In LH and FSH deficient women (hypogonadotrophic hypogonadism), the objective of GONAL-f
therapy in association with lutropin alfa is to develop a single mature Graafian follicle from which the
oocyte will be liberated after the administration of human chorionic gonadotropin (hCG). GONAL-f
should be given as a course of daily injections simultaneously with lutropin alfa. Since these patients
are amenorrhoeic and have low endogenous oestrogen secretion, treatment can commence at any time.
A recommended regimen commences at 75 IU of lutropin alfa daily with 75-150 IU FSH. Treatment
should be tailored to the individual patient’s response as assessed by measuring follicle size by
ultrasound and oestrogen response.
If an FSH dose increase is deemed appropriate, dose adaptation should preferably be after 7-14 day
intervals and preferably by 37.5-75 IU increments. It may be acceptable to extend the duration of
stimulation in any one cycle to up to 5 weeks.
When an optimal response is obtained, a single injection of 250 micrograms r-hCG or 5,000 IU up to
10,000 IU hCG should be administered 24-48 hours after the last GONAL-f and lutropin alfa
injections. The patient is recommended to have coitus on the day of, and on the day following, hCG
administration.
Alternatively, IUI may be performed.
Luteal phase support may be considered since lack of substances with luteotrophic activity (LH/hCG)
after ovulation may lead to premature failure of the corpus luteum.
If an excessive response is obtained, treatment should be stopped and hCG withheld. Treatment should
recommence in the next cycle at a dose of FSH lower than that of the previous cycle.
Men with hypogonadotrophic hypogonadism
GONAL-f should be given at a dose of 150 IU three times a week, concomitantly with hCG, for a
minimum of 4 months. If after this period, the patient has not responded, the combination treatment
may be continued; current clinical experience indicates that treatment for at least 18 months may be
necessary to achieve spermatogenesis.
There is no relevant use of GONAL-f in the elderly population. Safety and effectiveness of GONAL-f
in elderly patients have not been established.
Renal or hepatic impairment
Safety, efficacy and pharmacokinetics of GONAL-f in patients with renal or hepatic impairment have
not been established.
There is no relevant use of GONAL-f in the paediatric population.
GONAL-f is intended for subcutaneous administration. The first injection of GONAL-f should be
performed under direct medical supervision. Self-administration of GONAL-f should only be
performed by patients who are well motivated, adequately trained and have access to expert advice.
As GONAL-f multidose is intended for several injections, clear instructions should be provided to the
patients to avoid misuse of the multidose presentation.
Due to a local reactivity to benzyl alcohol, the same site of injection should not be used on consecutive
days.
Individual reconstituted vials should be for single patient use only.
For instructions on the reconstitution and administration of GONAL-f powder and solvent for solution
for injection see section 6.6 and the package leaflet.
• hypersensitivity to the active substance follitropin alfa, FSH or to any of the excipients
• tumours of the hypothalamus or pituitary gland
• ovarian enlargement or ovarian cyst not due to polycystic ovarian syndrome
• gynaecological haemorrhages of unknown aetiology
• ovarian, uterine or mammary carcinoma
GONAL-f must not be used when an effective response cannot be obtained, such as:
• primary ovarian failure
• malformations of sexual organs incompatible with pregnancy
• fibroid tumours of the uterus incompatible with pregnancy
• primary testicular insufficiency
4.4 Special warnings and precautions for use
GONAL-f is a potent gonadotrophic substance capable of causing mild to severe adverse reactions,
and should only be used by physicians who are thoroughly familiar with infertility problems and their
management.
Gonadotropin therapy requires a certain time commitment by physicians and supportive health
professionals, as well as the availability of appropriate monitoring facilities. In women, safe and
effective use of GONAL-f calls for monitoring of ovarian response with ultrasound, alone or
preferably in combination with measurement of serum oestradiol levels, on a regular basis. There may
be a degree of interpatient variability in response to FSH administration, with a poor response to FSH
in some patients and exaggerated response in others. The lowest effective dose in relation to the
treatment objective should be used in both men and women.
Patients with porphyria or a family history of porphyria should be closely monitored during treatment
with GONAL-f. Deterioration or a first appearance of this condition may require cessation of
treatment.
Before starting treatment, the couple’s infertility should be assessed as appropriate and putative
contraindications for pregnancy evaluated. In particular, patients should be evaluated for
hypothyroidism, adrenocortical deficiency, hyperprolactinemia and appropriate specific treatment
given.
Patients undergoing stimulation of follicular growth, whether as treatment for anovulatory infertility or
ART procedures, may experience ovarian enlargement or develop hyperstimulation. Adherence to
recommended GONAL-f dose and regimen of administration and careful monitoring of therapy will
minimise the incidence of such events. For accurate interpretation of the indices of follicle
development and maturation, the physician should be experienced in the interpretation of the relevant
tests.
In clinical trials, an increase of the ovarian sensitivity to GONAL-f was shown when administered
with lutropin alfa. If an FSH dose increase is deemed appropriate, dose adaptation should preferably
be at 7-14 day intervals and preferably with 37.5-75 IU increments.
No direct comparison of GONAL-f/LH versus human menopausal gonadotropin (hMG) has been
performed. Comparison with historical data suggests that the ovulation rate obtained with
GONAL-f/LH is similar to that obtained with hMG.
Ovarian Hyperstimulation Syndrome (OHSS)
A certain degree of ovarian enlargement is an expected effect of controlled ovarian stimulation. It is
more commonly seen in women with polycystic ovarian syndrome and usually regresses without
treatment.
In distinction to uncomplicated ovarian enlargement, OHSS is a condition that can manifest itself with
increasing degrees of severity. It comprises marked ovarian enlargement, high serum sex steroids, and
an increase in vascular permeability which can result in an accumulation of fluid in the peritoneal,
pleural and, rarely, in the pericardial cavities.
The following symptomatology may be observed in severe cases of OHSS: abdominal pain, abdominal
distension, severe ovarian enlargement, weight gain, dyspnoea, oliguria and gastrointestinal symptoms
including nausea, vomiting and diarrhoea. Clinical evaluation may reveal hypovolaemia,
haemoconcentration, electrolyte imbalances, ascites, haemoperitoneum, pleural effusions,
hydrothorax, or acute pulmonary distress. Very rarely, severe OHSS may be complicated by ovarian
torsion or thromboembolic events such as pulmonary embolism, ischaemic stroke or myocardial
infarction.
Independent risk factors for developing OHSS include polycystic ovarian syndrome high absolute or
rapidly rising serum oestradiol levels (e.g. > 900 pg/ml or > 3,300 pmol/l in anovulation;
> 3,000 pg/ml or > 11,000 pmol/l in ART) and large number of developing ovarian follicles (e.g.
> 3 follicles of ≥ 14 mm in diameter in anovulation; ≥ 20 follicles of ≥ 12 mm in diameter in ART).
Adherence to recommended GONAL-f dose and regimen of administration can minimise the risk of
ovarian hyperstimulation (see sections 4.2 and 4.8). Monitoring of stimulation cycles by ultrasound
scans as well as oestradiol measurements are recommended to early identify risk factors.
There is evidence to suggest that hCG plays a key role in triggering OHSS and that the syndrome may
be more severe and more protracted if pregnancy occurs. Therefore, if signs of ovarian
hyperstimulation occur such as serum oestradiol level > 5,500 pg/ml or > 20,200 pmol/l and/or ≥ 40
follicles in total, it is recommended that hCG be withheld and the patient be advised to refrain from
coitus or to use barrier contraceptive methods for at least 4 days. OHSS may progress rapidly (within
24 hours) or over several days to become a serious medical event. It most often occurs after hormonal
treatment has been discontinued and reaches its maximum at about seven to ten days following
treatment. Therefore patients should be followed for at least two weeks after hCG administration.
In ART, aspiration of all follicles prior to ovulation may reduce the occurrence of hyperstimulation.
Mild or moderate OHSS usually resolves spontaneously. If severe OHSS occurs, it is recommended
that gonadotropin treatment be stopped if still ongoing, and that the patient be hospitalised and
appropriate therapy be started.
In patients undergoing ovulation induction, the incidence of multiple pregnancy is increased compared
with natural conception. The majority of multiple conceptions are twins. Multiple pregnancy,
especially of high order, carries an increased risk of adverse maternal and perinatal outcomes.
To minimise the risk of multiple pregnancy, careful monitoring of ovarian response is recommended.
In patients undergoing ART procedures the risk of multiple pregnancy is related mainly to the number
of embryos replaced, their quality and the patient age.
The patients should be advised of the potential risk of multiple births before starting treatment.
The incidence of pregnancy loss by miscarriage or abortion is higher in patients undergoing
stimulation of follicular growth for ovulation induction or ART than following natural conception.
Women with a history of tubal disease are at risk of ectopic pregnancy, whether the pregnancy is
obtained by spontaneous conception or with fertility treatments. The prevalence of ectopic pregnancy
after ART, was reported to be higher than in the general population.
Reproductive system neoplasms
There have been reports of ovarian and other reproductive system neoplasms, both benign and
malignant, in women who have undergone multiple treatment regimens for infertility treatment. It is
not yet established whether or not treatment with gonadotropins increases the risk of these tumours in
infertile women.
The prevalence of congenital malformations after ART may be slightly higher than after spontaneous
conceptions. This is thought to be due to differences in parental characteristics (e.g. maternal age,
sperm characteristics) and multiple pregnancies.
In women with recent or ongoing thromboembolic disease or women with generally recognised risk
factors for thrombo-embolic events, such as personal or family history, treatment with gonadotropins
may further increase the risk for aggravation or occurrence of such events. In these women, the
benefits of gonadotropin administration need to be weighed against the risks. It should be noted
however that pregnancy itself as well as OHSS also carry an increased risk of thrombo-embolic
events.
Elevated endogenous FSH levels are indicative of primary testicular failure. Such patients are
unresponsive to GONAL-f/hCG therapy. GONAL-f should not be used when an effective response
cannot be obtained.
Semen analysis is recommended 4 to 6 months after the beginning of treatment as part of the
assessment of the response.
GONAL-f contains less than 1 mmol sodium (23 mg) per dose, i.e. essentially “sodium-free”.
4.5 Interaction with other medicinal products and other forms of interaction
Concomitant use of GONAL-f with other medicinal products used to stimulate ovulation (e.g. hCG,
clomiphene citrate) may potentiate the follicular response, whereas concurrent use of a GnRH agonist
or antagonist to induce pituitary desensitisation may increase the dose of GONAL-f needed to elicit an
adequate ovarian response. No other clinically significant medicinal product interaction has been
reported during GONAL-f therapy.
4.6 Fertility, pregnancy and lactation
Pregnancy
There is no indication for use of GONAL-f during pregnancy. Data on a limited number of exposed
pregnancies (less than 300 pregnancy outcomes) indicate no malformative or feto/neonatal toxicity of
follitropin alfa.
No teratogenic effect has been observed in animal studies (see section 5.3).
In case of exposure during pregnancy, clinical data are not sufficient to exclude a teratogenic effect of
GONAL-f.
Breastfeeding
GONAL-f is not indicated during breastfeeding.
Fertility
GONAL-f is indicated for use in infertility (see section 4.1).
4.7 Effects on ability to drive and use machines
GONAL-f is expected to have no or negligible influence on the ability to drive and use machines.
The most commonly reported adverse reactions are headache, ovarian cysts and local injection site
reactions (e.g. pain, erythema, haematoma, swelling and/or irritation at the site of injection).
Mild or moderate ovarian hyperstimulation syndrome (OHSS) have been commonly reported and
should be considered as an intrinsic risk of the stimulation procedure. Severe OHSS is uncommon (see
section 4.4).
Thromboembolism may occur very rarely, usually associated with severe OHSS (see section 4.4).
The following definitions apply to the frequency terminology used hereafter:
Very common (≥ 1/10)
Common (≥ 1/100 to < 1/10)
Uncommon (≥ 1/1,000 to < 1/100)
Rare (≥ 1/10,000 to < 1/1,000)
Very rare (< 1/10,000)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Nervous system disorders
Very common: Headache
Vascular disorders
Very rare: Thromboembolism, usually associated with severe OHSS (see section 4.4)
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Gastrointestinal disorders
Common: Abdominal pain, abdominal distension, abdominal discomfort, nausea, vomiting,
diarrhoea
Reproductive system and breast disorders
Very common: Ovarian cysts
Common:
Mild or moderate OHSS (including associated symptomatology)
Complication of severe OHSS
Severe OHSS (including associated symptomatology) (see section 4.4)
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Skin and subcutaneous tissue disorders
Common: Acne
Reproductive system and breast disorders
Common: Gynaecomastia,Varicocele
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Investigations
Common: Weight gain
The effects of an overdose of GONAL-f are unknown, nevertheless, there is a possibility that OHSS
may occur (see section 4.4).
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: Sex hormones and modulators of the genital systems, gonadotropins,
ATC code: G03GA05.
In women, the most important effect resulting from parenteral administration of FSH is the
development of mature Graafian follicles.
In women with anovulation, the object of GONAL-f therapy
is to develop a single mature Graafian follicle from which the ovum will be liberated after the
administration of hCG.
Clinical efficacy and safety in women
In clinical trials, patients with severe FSH and LH deficiency were defined by an endogenous serum
LH level < 1.2 IU/l as measured in a central laboratory. However, it should be taken into account that
there are variations between LH measurements performed in different laboratories.
In clinical studies comparing r-hFSH (follitropin alfa) and urinary FSH in ART (see table below) and
in ovulation induction, GONAL-f was more potent than urinary FSH in terms of a lower total dose and
a shorter treatment period needed to trigger follicular maturation.
In ART, GONAL-f at a lower total dose and shorter treatment period than urinary FSH, resulted in a
higher number of oocytes retrieved when compared to urinary FSH.
Table: Results of study GF 8407 (randomised parallel group study comparing efficacy and safety of
GONAL-f with urinary FSH in assisted reproduction technologies)
Number of oocytes retrieved
Days of FSH stimulation required
Total dose of FSH required (number
of FSH 75 IU ampoules)
Need to increase the dose (%) 56.2 85.3
Differences between the 2 groups were statistically significant (p< 0.05) for all criteria listed.
Clinical efficacy and safety in men
In men deficient in FSH, GONAL-f administered concomitantly with hCG for at least 4 months
induces spermatogenesis.









5.2 Pharmacokinetic properties
Following intravenous administration, follitropin alfa is distributed to the extracellular fluid space with
an initial half-life of around 2 hours and eliminated from the body with a terminal half-life of about
one day. The steady state volume of distribution and total clearance are 10 l and 0.6 l/h, respectively.
One-eighth of the follitropin alfa dose is excreted in the urine.
Following subcutaneous administration, the absolute bioavailability is about 70 %. Following repeated
administration, follitropin alfa accumulates 3-fold achieving a steady-state within 3-4 days. In women
whose endogenous gonadotropin secretion is suppressed, follitropin alfa has nevertheless been shown
to effectively stimulate follicular development and steroidogenesis, despite unmeasurable LH levels.
5.3 Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of single and
repeated dose toxicity and genotoxicity additional to that already stated in other sections of this SmPC.
In rabbits, the formulation reconstituted with 0.9 % benzyl alcohol and 0.9 % benzyl alcohol alone,
both resulted in a slight haemorrhage and subacute inflammation after single subcutaneous injection or
mild inflammatory and degenerative changes after single intramuscular injection respectively.
Impaired fertility has been reported in rats exposed to pharmacological doses of follitropin alfa
(≥ 40 IU/kg/day) for extended periods, through reduced fecundity.
Given in high doses (≥ 5 IU/kg/day) follitropin alfa caused a decrease in the number of viable foetuses
without being a teratogen, and dystocia similar to that observed with urinary Menopausal
Gonadotropin (hMG). However, since GONAL-f is not indicated in pregnancy, these data are of
limited clinical relevance.
PHARMACEUTICAL PARTICULARS
Sucrose
Sodium dihydrogen phosphate monohydrate
Disodium phosphate dihydrate
Phosphoric acid, concentrated
Sodium hydroxide
Water for injections
Benzyl alcohol
In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal
products.
The reconstituted solution is stable for 28 days at or below 25°C.
6.4 Special precautions for storage
Prior to reconstitution, do not store above 25°C. Store in the original package, in order to protect from
light.
After reconstitution, do not store above 25°C. Do not freeze. Store in the original container, in order to
protect from light.
6.5 Nature and contents of container
GONAL f is presented as a powder and solvent for injection. The powder is presented in 3 ml vials
(Type I glass), with rubber stopper (bromobutyl rubber) and aluminium flip-off cap. The solvent for
reconstitution is presented in 2 ml pre-filled syringes (Type I glass) with a rubber stopper. The
administration syringes made of polypropylene with a stainless steel pre-fixed needle are also
provided.
The medicinal product is supplied as a pack of 1 vial of powder with 1 pre-filled syringe of solvent for
reconstitution and 15 disposable syringes for administration graduated in FSH units.
6.6 Special precautions for disposal and other handling
GONAL-f 1050 IU/1.75 ml (77 micrograms/1.75 ml) must be reconstituted with the 2 ml solvent
provided before use.
GONAL-f 1050 IU/1.75 ml (77 micrograms/1.75 ml) preparation must not be reconstituted with any
other GONAL-f containers.
The solvent pre-filled syringe provided should be used for reconstitution only and then disposed of in
accordance with local requirements. A set of administration syringes graduated in FSH units is
supplied in the GONAL-f multidose box. Alternatively, a 1 ml syringe, graduated in ml, with pre-fixed
needle for subcutaneous administration could be used (see section “How to prepare and use the
GONAL-f powder and solvent” in the package leaflet).
The reconstituted solution should not be administered if it contains particles or is not clear.Any unused
medicinal product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
Merck Serono Europe Ltd.
56 Marsh Wall
London E14 9TP
United Kingdom
MARKETING AUTHORISATION NUMBER
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 20 October 1995.
Date of last renewal: 20 October 2005.
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency http://www.ema.europa.eu
NAME OF THE MEDICINAL PRODUCT
GONAL-f 450 IU/0.75 ml (33 micrograms/0.75 ml) powder and solvent for solution for injection.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each vial contains 33 micrograms of follitropin alfa* equivalent to 450 IU. Each ml of the
reconstituted solution contains 600 IU.
* recombinant human follicle stimulating hormone (r-hFSH) produced in Chinese Hamster Ovary
(CHO) cells by recombinant DNA technology.
For a full list of excipients, see section 6.1.
Powder and solvent for solution for injection.
Appearance of the powder: white lyophilised pellet.
Appearance of the solvent: clear colourless solution.
The pH of the reconstituted solution is 6.5-7.5.
4.1 Therapeutic indications
• Anovulation (including polycystic ovarian syndrome) in women who have been unresponsive to
treatment with clomiphene citrate.
• Stimulation of multifollicular development in women undergoing superovulation for assisted
reproductive technologies (ART) such as
in vitro
fertilisation (IVF), gamete intra-fallopian
transfer and zygote intra-fallopian transfer.
• GONAL-f in association with a luteinising hormone (LH) preparation is recommended for the
stimulation of follicular development in women with severe LH and FSH deficiency. In clinical
trials these patients were defined by an endogenous serum LH level < 1.2 IU/l.
• GONAL-f is indicated for the stimulation of spermatogenesis in men who have congenital or
acquired hypogonadotrophic hypogonadism with concomitant human Chorionic Gonadotropin
(hCG) therapy.
4.2 Posology and method of administration
Treatment with GONAL-f should be initiated under the supervision of a physician experienced in the
treatment of fertility disorders.
The dose recommendations given for GONAL-f are those in use for urinary FSH. Clinical assessment
of GONAL-f indicates that its daily doses, regimens of administration, and treatment monitoring
procedures should not be different from those currently used for urinary FSH-containing medicinal
products. It is advised to adhere to the recommended starting doses indicated below.
Comparative clinical studies have shown that on average patients require a lower cumulative dose and
shorter treatment duration with GONAL-f compared with urinary FSH. Therefore, it is considered
appropriate to give a lower total dose of GONAL-f than generally used for urinary FSH, not only in
order to optimise follicular development but also to minimise the risk of unwanted ovarian
hyperstimulation. See section 5.1.
Bioequivalence has been demonstrated between equivalent doses of the monodose presentation and
the multidose presentation of GONAL-f.
The following table states the volume to be administered to deliver the prescribed dose:
Volume to be injected (ml)
The next injection should be done at the same time the next day.
Women with anovulation (including polycystic ovarian syndrome)
GONAL-f may be given as a course of daily injections. In menstruating women treatment should
commence within the first 7 days of the menstrual cycle.
A commonly used regimen commences at 75-150 IU FSH daily and is increased preferably by 37.5 or
75 IU at 7 or preferably 14 day intervals if necessary, to obtain an adequate, but not excessive,
response. Treatment should be tailored to the individual patient’s response as assessed by measuring
follicle size by ultrasound and/or oestrogen secretion. The maximal daily dose is usually not higher
than 225 IU FSH. If a patient fails to respond adequately after 4 weeks of treatment, that cycle should
be abandoned and the patient should undergo further evaluation after which she may recommence
treatment at a higher starting dose than in the abandoned cycle.
When an optimal response is obtained, a single injection of 250 micrograms recombinant human
choriogonadotropin alfa (r-hCG) or 5,000 IU, up to 10,000 IU hCG should be administered
24-48 hours after the last GONAL-f injection. The patient is recommended to have coitus on the day
of, and the day following, hCG administration. Alternatively intrauterine insemination (IUI) may be
performed.
If an excessive response is obtained, treatment should be stopped and hCG withheld (see section 4.4).
Treatment should recommence in the next cycle at a dose lower than that of the previous cycle.
Women undergoing ovarian stimulation for multiple follicular development prior to in vitro
fertilisation or other assisted reproductive technologies.
A commonly used regimen for superovulation involves the administration of 150-225 IU of GONAL-f
daily, commencing on days 2 or 3 of the cycle. Treatment is continued until adequate follicular
development has been achieved (as assessed by monitoring of serum oestrogen concentrations and/or
ultrasound examination), with the dose adjusted according to the patient’s response, to usually not










higher than 450 IU daily. In general adequate follicular development is achieved on average by the
tenth day of treatment (range 5 to 20 days).
A single injection of 250 micrograms r-hCG or 5,000 IU up to 10,000 IU hCG is administered
24-48 hours after the last GONAL-f injection to induce final follicular maturation.
Down-regulation with a gonadotropin-releasing hormone (GnRH) agonist or antagonist is now
commonly used in order to suppress the endogenous LH surge and to control tonic levels of LH. In a
commonly used protocol, GONAL-f is started approximately 2 weeks after the start of agonist
treatment, both being continued until adequate follicular development is achieved. For example,
following two weeks of treatment with an agonist, 150-225 IU GONAL-f are administered for the first
7 days. The dose is then adjusted according to the ovarian response.
Overall experience with IVF indicates that in general the treatment success rate remains stable during
the first four attempts and gradually declines thereafter.
Women with anovulation resulting from severe LH and FSH deficiency.
In LH and FSH deficient women (hypogonadotrophic hypogonadism), the objective of GONAL-f
therapy in association with lutropin alfa is to develop a single mature Graafian follicle from which the
oocyte will be liberated after the administration of human chorionic gonadotropin (hCG). GONAL-f
should be given as a course of daily injections simultaneously with lutropin alfa. Since these patients
are amenorrhoeic and have low endogenous oestrogen secretion, treatment can commence at any time.
A recommended regimen commences at 75 IU of lutropin alfa daily with 75-150 IU FSH. Treatment
should be tailored to the individual patient’s response as assessed by measuring follicle size by
ultrasound and oestrogen response.
If an FSH dose increase is deemed appropriate, dose adaptation should preferably be after 7-14 day
intervals and preferably by 37.5-75 IU increments. It may be acceptable to extend the duration of
stimulation in any one cycle to up to 5 weeks.
When an optimal response is obtained, a single injection of 250 micrograms r-hCG or 5,000 IU up to
10,000 IU hCG should be administered 24-48 hours after the last GONAL-f and lutropin alfa
injections. The patient is recommended to have coitus on the day of, and on the day following, hCG
administration.
Alternatively, IUI may be performed.
Luteal phase support may be considered since lack of substances with luteotrophic activity (LH/hCG)
after ovulation may lead to premature failure of the corpus luteum.
If an excessive response is obtained, treatment should be stopped and hCG withheld. Treatment should
recommence in the next cycle at a dose of FSH lower than that of the previous cycle.
Men with hypogonadotrophic hypogonadism
GONAL-f should be given at a dose of 150 IU three times a week, concomitantly with hCG, for a
minimum of 4 months. If after this period, the patient has not responded, the combination treatment
may be continued; current clinical experience indicates that treatment for at least 18 months may be
necessary to achieve spermatogenesis.
There is no relevant use of GONAL-f in the elderly population. Safety and effectiveness of GONAL-f
in elderly patients have not been established.
Renal or hepatic impairment
Safety, efficacy and pharmacokinetics of GONAL-f in patients with renal or hepatic impairment have
not been established.
There is no relevant use of GONAL-f in the paediatric population.
GONAL-f is intended for subcutaneous administration. The first injection of GONAL--f should be
performed under direct medical supervision. Self-administration of GONAL-f should only be
performed by patients who are well motivated, adequately trained and have access to expert advice.
As GONAL-f multidose is intended for several injections, clear instructions should be provided to the
patients to avoid misuse of the multidose presentation.
Due to a local reactivity to benzyl alcohol, the same site of injection should not be used on consecutive
days.
Individual reconstituted vials should be for single patient use only.
For instructions on the reconstitution and administration of GONAL-f powder and solvent for solution
for injection see section 6.6 and the package leaflet.
• hypersensitivity to the active substance follitropin alfa, FSH or to any of the excipients
• tumours of the hypothalamus or pituitary gland
• ovarian enlargement or ovarian cyst not due to polycystic ovarian syndrome
• gynaecological haemorrhages of unknown aetiology
• ovarian, uterine or mammary carcinoma
GONAL-f must not be used when an effective response cannot be obtained, such as:
• primary ovarian failure
• malformations of sexual organs incompatible with pregnancy
• fibroid tumours of the uterus incompatible with pregnancy
• primary testicular insufficiency
4.4 Special warnings and precautions for use
GONAL-f is a potent gonadotrophic substance capable of causing mild to severe adverse reactions,
and should only be used by physicians who are thoroughly familiar with infertility problems and their
management.
Gonadotropin therapy requires a certain time commitment by physicians and supportive health
professionals, as well as the availability of appropriate monitoring facilities. In women, safe and
effective use of GONAL-f calls for monitoring of ovarian response with ultrasound, alone or
preferably in combination with measurement of serum oestradiol levels, on a regular basis. There may
be a degree of interpatient variability in response to FSH administration, with a poor response to FSH
in some patients and exaggerated response in others. The lowest effective dose in relation to the
treatment objective should be used in both men and women.
Patients with porphyria or a family history of porphyria should be closely monitored during treatment
with GONAL-f. Deterioration or a first appearance of this condition may require cessation of
treatment.
Before starting treatment, the couple’s infertility should be assessed as appropriate and putative
contraindications for pregnancy evaluated. In particular, patients should be evaluated for
hypothyroidism, adrenocortical deficiency, hyperprolactinemia and appropriate specific treatment
given.
Patients undergoing stimulation of follicular growth, whether as treatment for anovulatory infertility or
ART procedures, may experience ovarian enlargement or develop hyperstimulation. Adherence to
recommended GONAL-f dose and regimen of administration and careful monitoring of therapy will
minimise the incidence of such events. For accurate interpretation of the indices of follicle
development and maturation, the physician should be experienced in the interpretation of the relevant
tests.
In clinical trials, an increase of the ovarian sensitivity to GONAL-f was shown when administered
with lutropin alfa. If an FSH dose increase is deemed appropriate, dose adaptation should preferably
be at 7-14 day intervals and preferably with 37.5-75 IU increments.
No direct comparison of GONAL-f/LH versus human menopausal gonadotropin (hMG) has been
performed. Comparison with historical data suggests that the ovulation rate obtained with
GONAL-f/LH is similar to that obtained with hMG.
Ovarian Hyperstimulation Syndrome (OHSS)
A certain degree of ovarian enlargement is an expected effect of controlled ovarian stimulation. It is
more commonly seen in women with polycystic ovarian syndrome and usually regresses without
treatment.
In distinction to uncomplicated ovarian enlargement, OHSS is a condition that can manifest itself with
increasing degrees of severity. It comprises marked ovarian enlargement, high serum sex steroids, and
an increase in vascular permeability which can result in an accumulation of fluid in the peritoneal,
pleural and, rarely, in the pericardial cavities.
The following symptomatology may be observed in severe cases of OHSS: abdominal pain, abdominal
distension, severe ovarian enlargement, weight gain, dyspnoea, oliguria and gastrointestinal symptoms
including nausea, vomiting and diarrhoea. Clinical evaluation may reveal hypovolaemia,
haemoconcentration, electrolyte imbalances, ascites, haemoperitoneum, pleural effusions,
hydrothorax, or acute pulmonary distress. Very rarely, severe OHSS may be complicated by ovarian
torsion or thromboembolic events such as pulmonary embolism, ischaemic stroke or myocardial
infarction.
Independent risk factors for developing OHSS include polycystic ovarian syndrome high absolute or
rapidly rising serum oestradiol levels (e.g. > 900 pg/ml or > 3,300 pmol/l in anovulation;
> 3,000 pg/ml or > 11,000 pmol/l in ART) and large number of developing ovarian follicles (e.g.
> 3 follicles of ≥ 14 mm in diameter in anovulation; ≥ 20 follicles of ≥ 12 mm in diameter in ART).
Adherence to recommended GONAL-f dose and regimen of administration can minimise the risk of
ovarian hyperstimulation (see sections 4.2 and 4.8). Monitoring of stimulation cycles by ultrasound
scans as well as oestradiol measurements are recommended to early identify risk factors.
There is evidence to suggest that hCG plays a key role in triggering OHSS and that the syndrome may
be more severe and more protracted if pregnancy occurs. Therefore, if signs of ovarian
hyperstimulation occur such as serum oestradiol level > 5,500 pg/ml or > 20,200 pmol/l and/or ≥ 40
follicles in total, it is recommended that hCG be withheld and the patient be advised to refrain from
coitus or to use barrier contraceptive methods for at least 4 days. OHSS may progress rapidly (within
24 hours) or over several days to become a serious medical event. It most often occurs after hormonal
treatment has been discontinued and reaches its maximum at about seven to ten days following
treatment. Therefore patients should be followed for at least two weeks after hCG administration.
In ART, aspiration of all follicles prior to ovulation may reduce the occurrence of hyperstimulation.
Mild or moderate OHSS usually resolves spontaneously. If severe OHSS occurs, it is recommended
that gonadotropin treatment be stopped if still ongoing, and that the patient be hospitalised and
appropriate therapy be started.
In patients undergoing ovulation induction, the incidence of multiple pregnancy is increased compared
with natural conception. The majority of multiple conceptions are twins. Multiple pregnancy,
especially of high order, carries an increased risk of adverse maternal and perinatal outcomes.
To minimise the risk of multiple pregnancy, careful monitoring of ovarian response is recommended.
In patients undergoing ART procedures the risk of multiple pregnancy is related mainly to the number
of embryos replaced, their quality and the patient age.
The patients should be advised of the potential risk of multiple births before starting treatment.
The incidence of pregnancy loss by miscarriage or abortion is higher in patients undergoing
stimulation of follicular growth for ovulation induction or ART than following natural conception.
Women with a history of tubal disease are at risk of ectopic pregnancy, whether the pregnancy is
obtained by spontaneous conception or with fertility treatments. The prevalence of ectopic pregnancy
after ART, was reported to be higher than in the general population.
Reproductive system neoplasms
There have been reports of ovarian and other reproductive system neoplasms, both benign and
malignant, in women who have undergone multiple treatment regimens for infertility treatment. It is
not yet established whether or not treatment with gonadotropins increases the risk of these tumours in
infertile women.
The prevalence of congenital malformations after ART may be slightly higher than after spontaneous
conceptions. This is thought to be due to differences in parental characteristics (e.g. maternal age,
sperm characteristics) and multiple pregnancies.
In women with recent or ongoing thromboembolic disease or women with generally recognised risk
factors for thrombo-embolic events, such as personal or family history, treatment with gonadotropins
may further increase the risk for aggravation or occurrence of such events. In these women, the
benefits of gonadotropin administration need to be weighed against the risks. It should be noted
however that pregnancy itself as well as OHSS also carry an increased risk of thrombo-embolic
events.
Elevated endogenous FSH levels are indicative of primary testicular failure. Such patients are
unresponsive to GONAL-f/hCG therapy. GONAL-f should not be used when an effective response
cannot be obtained.
Semen analysis is recommended 4 to 6 months after the beginning of treatment as part of the
assessment of the response.
GONAL-f contains less than 1 mmol sodium (23 mg) per dose, i.e. essentially “sodium-free”.
4.5 Interaction with other medicinal products and other forms of interaction
Concomitant use of GONAL-f with other medicinal products used to stimulate ovulation (e.g. hCG,
clomiphene citrate) may potentiate the follicular response, whereas concurrent use of a GnRH agonist
or antagonist to induce pituitary desensitisation may increase the dose of GONAL-f needed to elicit an
adequate ovarian response. No other clinically significant medicinal product interaction has been
reported during GONAL-f therapy.
4.6 Fertility, pregnancy and lactation
Pregnancy
There is no indication for use of GONAL-f during pregnancy. Data on a limited number of exposed
pregnancies (less than 300 pregnancy outcomes) indicate no malformative or feto/neonatal toxicity of
follitropin alfa.
No teratogenic effect has been observed in animal studies (see section 5.3).
In case of exposure during pregnancy, clinical data are not sufficient to exclude a teratogenic effect of
GONAL-f.
Breastfeeding
GONAL-f is not indicated during breastfeeding.
Fertility
GONAL-f is indicated for use in infertility (see section 4.1).
4.7 Effects on ability to drive and use machines
GONAL-f is expected to have no or negligible influence on the ability to drive and use machines.
The most commonly reported adverse reactions are headache, ovarian cysts and local injection site
reactions (e.g. pain, erythema, haematoma, swelling and/or irritation at the site of injection).
Mild or moderate ovarian hyperstimulation syndrome (OHSS) have been commonly reported and
should be considered as an intrinsic risk of the stimulation procedure. Severe OHSS is uncommon (see
section 4.4).
Thromboembolism may occur very rarely, usually associated with severe OHSS (see section 4.4).
The following definitions apply to the frequency terminology used hereafter:
Very common (≥ 1/10)
Common (≥ 1/100 to < 1/10)
Uncommon (≥ 1/1,000 to < 1/100)
Rare (≥ 1/10,000 to < 1/1,000)
Very rare (< 1/10,000)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Nervous system disorders
Very common: Headache
Vascular disorders
Very rare: Thromboembolism, usually associated with severe OHSS (see section 4.4)
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Gastrointestinal disorders
Common: Abdominal pain, abdominal distension, abdominal discomfort, nausea, vomiting,
diarrhoea
Reproductive system and breast disorders
Very common: Ovarian cysts
Common:
Severe OHSS (including associated symptomatology) (see section 4.4)
Complication of severe OHSS
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Immune system disorders
Very rare: Mild to severe hypersensitivity reactions including anaphylactic reactions and shock
Respiratory, thoracic and mediastinal disorders
Very rare: Exacerbation or aggravation of asthma
Skin and subcutaneous tissue disorders
Common: Acne
Reproductive system and breast disorders
Common: Gynaecomastia,Varicocele
General disorders and administration site conditions
Very common: Injection site reactions (e.g. pain, erythema, haematoma, swelling and/or irritation
at the site of injection)
Investigations
Common: Weightgain
Mild or moderate OHSS (including associated symptomatology)
The effects of an overdose of GONAL-f are unknown, nevertheless, there is a possibility that OHSS
may occur (see section 4.4).
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: Sex hormones and modulators of the genital systems, gonadotropins,
ATC code: G03GA05.
In women, the most important effect resulting from parenteral administration of FSH is the
development of mature Graafian follicles.
In women with anovulation, the object of GONAL-f therapy
is to develop a single mature Graafian follicle from which the ovum will be liberated after the
administration of hCG.
Clinical efficacy and safety in women
In clinical trials, patients with severe FSH and LH deficiency were defined by an endogenous serum
LH level < 1.2 IU/l as measured in a central laboratory. However, it should be taken into account that
there are variations between LH measurements performed in different laboratories.
In clinical studies comparing r-hFSH (follitropin alfa) and urinary FSH in ART (see table below) and
in ovulation induction, GONAL-f was more potent than urinary FSH in terms of a lower total dose and
a shorter treatment period needed to trigger follicular maturation.
In ART, GONAL-f at a lower total dose and shorter treatment period than urinary FSH, resulted in a
higher number of oocytes retrieved when compared to urinary FSH.
Table: Results of study GF 8407 (randomised parallel group study comparing efficacy and safety of
GONAL-f with urinary FSH in assisted reproduction technologies)
Number of oocytes retrieved
Days of FSH stimulation required
Total dose of FSH required (number
of FSH 75 IU ampoules)
Need to increase the dose (%) 56.2 85.3
Differences between the 2 groups were statistically significant (p< 0.05) for all criteria listed.
Clinical efficacy and safety in men
In men deficient in FSH, GONAL-f administered concomitantly with hCG for at least 4 months
induces spermatogenesis.
5.2 Pharmacokinetic properties
Following intravenous administration, follitropin alfa is distributed to the extracellular fluid space with
an initial half-life of around 2 hours and eliminated from the body with a terminal half-life of about
one day. The steady state volume of distribution and total clearance are 10 l and 0.6 l/h, respectively.
One-eighth of the follitropin alfa dose is excreted in the urine.
Following subcutaneous administration, the absolute bioavailability is about 70 %. Following repeated
administration, follitropin alfa accumulates 3-fold achieving a steady-state within 3-4 days. In women









whose endogenous gonadotropin secretion is suppressed, follitropin alfa has nevertheless been shown
to effectively stimulate follicular development and steroidogenesis, despite unmeasurable LH levels.
5.3 Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of single and
repeated dose toxicity and genotoxicity additional to that already stated in other sections of this SmPC.
In rabbits, the formulation reconstituted with 0.9 % benzyl alcohol and 0.9 % benzyl alcohol alone,
both resulted in a slight haemorrhage and subacute inflammation after single subcutaneous injection or
mild inflammatory and degenerative changes after single intramuscular injection respectively.
Impaired fertility has been reported in rats exposed to pharmacological doses of follitropin alfa
(≥ 40 IU/kg/day) for extended periods, through reduced fecundity.
Given in high doses (≥ 5 IU/kg/day) follitropin alfa caused a decrease in the number of viable foetuses
without being a teratogen, and dystocia similar to that observed with urinary Menopausal
Gonadotropin (hMG). However, since GONAL-f is not indicated in pregnancy, these data are of
limited clinical relevance.
PHARMACEUTICAL PARTICULARS
Sucrose
Sodium dihydrogen phosphate monohydrate
Disodium phosphate dihydrate
Phosphoric acid, concentrated
Sodium hydroxide
Water for injections
Benzyl alcohol
In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal
products.
The reconstituted solution is stable for 28 days at or below 25°C.
6.4 Special precautions for storage
Prior to reconstitution, do not store above 25°C. Store in the original package, in order to protect from
light.
After reconstitution, do not store above 25°C. Do not freeze. Store in the original container, in order to
protect from light.
6.5 Nature and contents of container
GONAL f is presented as a powder and solvent for injection. The powder is presented in 3 ml vials
(Type I glass), with rubber stopper (bromobutyl rubber) and aluminium flip-off cap. The solvent for
reconstitution is presented in 1 ml pre-filled syringes (Type I glass) with a rubber stopper. The
administration syringes made of polypropylene with a stainless steel pre-fixed needle are also
provided.
The medicinal product is supplied as a pack of 1 vial of powder with 1 pre-filled syringe of solvent for
reconstitution and 6 disposable syringes for administration graduated in FSH units.
6.6 Special precautions for disposal and other handling
GONAL-f 450 IU/0.75 ml (33 micrograms/0.75 ml) must be reconstituted with the 1 ml solvent
provided before use.
GONAL-f 450 IU/0.75 ml (33 micrograms/0.75 ml) preparation must not be reconstituted with any
other GONAL-f containers.
The solvent pre-filled syringe provided should be used for reconstitution only and then disposed of in
accordance with local requirements. A set of administration syringes graduated in FSH units is
supplied in the GONAL-f multidose box. Alternatively, a 1 ml syringe, graduated in ml, with pre-fixed
needle for subcutaneous administration could be used (see section “How to prepare and use the
GONAL-f powder and solvent” in the package leaflet).
The reconstituted solution should not be administered if it contains particles or is not clear.Any unused
medicinal product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
Merck Serono Europe Ltd.
56 Marsh Wall
London E14 9TP
United Kingdom
MARKETING AUTHORISATION NUMBER
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 20 October 1995.
Date of last renewal: 20 October 2005.
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency http://www.ema.europa.eu
• The active substance is follitropin alfa.
• There are 600 IU (44 micrograms) of follitropin alfa in each millilitre of liquid. Each pre-filled
pen with multidose cartridge delivers 900 IU (66 micrograms) in 1.5 ml.
• The other ingredients are poloxamer 188, sucrose, methionine, sodium dihydrogen phosphate
monohydrate, disodium phosphate dihydrate, m-cresol, concentrated phosphoric acid, sodium
hydroxide and water for injections.
What GONAL-f looks like and contents of the pack
• GONAL-f is presented as a clear, colourless liquid for injection in a pre-filled pen.
• It is supplied in packs with 1 pre-filled pen and 14 disposable needles .
Marketing Authorisation Holder
Merck Serono Europe Limited, 56 Marsh Wall, London E14 9TP, United Kingdom.
Merck Serono S.p.A., Via delle Magnolie 15, I-70026 Modugno (Bari), Italy.
For any information about this medicine, please contact the local representative of the Marketing
Authorisation Holder.
België/Belgique/Belgien
MERCK NV/SA
Brusselsesteenweg 288
B-3090 Overijse
Tél/Tel: +32-2-686 07 11
Luxembourg/Luxemburg
MERCK NV/SA
Brusselsesteenweg 288
B-3090 Overijse, Belgique/Belgien
Tél/Tel: +32-2-686 07 11
България
Мерк България" ЕАД
Бул. Проф. Цветан Лазаров“ 83
София 1582
България
Teл: +359 28075 111
Magyarország
Merck Kft.
Bocskai út 134-146.
H-1113 Budapest
Tel: +36-1-463-8100
Česká republika
Merck spol. s r.o
Na Hřebenech II. 1718/10
CZ-140 00 Praha 4
Tel. +420 272084211
Malta
Cherubino Ltd
Delf Building
Sliema Road
MT-GZR 06 Gzira Malta
Tel: +356-21-343270/1/2/3/4
Danmark
E. Merck AB
Strandvejen 102 B, 4th
DK-2900 Hellerup
Tlf: +45 35253550
Nederland
Merck BV
Tupolevlaan 41-61
NL-1119 NW Schiphol-Rijk
Tel: +31-20-6582800
Deutschland
Merck Serono GmbH
Alsfelder Straße 17
D-64289 Darmstadt
Tel: +49-6151-6285-0
Norge
Merck Serono Norge
Luhrtoppen 2
N-1470 Lørenskog
Tlf: +47 67 90 35 90
Eesti
Merck Serono OÜ
Ahtri 12,
EE-10151, Tallinn
Tel: +372 6116220
Österreich
Merck GesmbH.
Zimbagasse 5
A-1147 Wien
Tel: +43 1 57600-0
Ελλάδα
Merck A.E.
Κηφισίας 41-45, Κτίριο Β
GR-151 23 Μαρούσι
Αθήνα
Tηλ: +30-210-61 65 100
Polska
Merck Sp. z o.o.
Al. Jerozolimskie 178
PL-02-486 Warszawa
Tel.: +48 22 53 59 700
España
Merck S.L.
María de Molina, 40
E-28006 Madrid
Línea de Información: 900 200 400
Tel: +34-91-745 44 00
Portugal
Merck, s.a.
Rua Alfredo da Silva, 3-C
P-1300-040 Lisboa
Tel: +351-21-361 35 00
France
Merck Serono s.a.s.
37, rue Saint-Romain
F-69379 Lyon cedex 08
Tél.: +33-4-72 78 25 25
Numéro vert : 0 800 888 024
România
MERCK d.o.o.,
Dunajska cesta 119
SI-1000 Lubliana, Slovenia
Tel: +386 1 560 3 800
Ireland
Merck Serono Ltd
Bedfont Cross, Stanwell Road
Feltham, Middlesex TW14 8NX
United Kingdom
Tel: +44-20 8818 7200
Slovenija
MERCK d.o.o.
Dunajska cesta 119
SI-1000 Ljubljana
Tel: +386 1 560 3 800
Ísland
Icepharma hf
Lynghálsi 13
IS-110 Reykjavík
Tel: + 354 540 8000
Slovenská republika
Merck spol. s r.o.
Tuhovská 3
SK-831 06 Bratislava
Tel: + 421 2 49 267 111
Italia
Merck Serono S.p.A.
Via Casilina 125
I-00176 Roma
Tel: +39-06-70 38 41
Suomi/Finland
Merck Oy
Pihatörmä 1 C
FIN-02240 Espoo
Puh/Tel: +358-9-8678 700
Κύπρος
Χρ. Γ. Παπαλοϊζου Λτδ
Λεωφόρος Κιλκίς 35,
CY-2234 Λατσιά, Λευκωσία
Τηλ.: +357 22490305
Sverige
E. Merck AB
S-195 87 Stockholm
Tel: +46-8-562 445 00
Latvija
Merck Serono SIA
Duntes iela 23A
LV-1005, Rīga
Tel: +371 67152500
United Kingdom
Merck Serono Ltd
Bedfont Cross, Stanwell Road
Feltham, Middlesex TW14 8NX- UK
Tel: +44-20 8818 7200
Lietuva
Merck Serono UAB
Savanoriu pr. 192,
LT-44151 Kaunas
Tel: +370 37320603
This leaflet was last approved in
Detailed information on this medicine is available on the European Medicines Agency web site:
http://www.ema.europa.eu
--------------------------------------------------------------------------------------------------
HOW TO USE THE GONAL-f PRE-FILLED PEN
• This section tells you how to use your pen.
• Before starting to use your pen, please read these instructions the whole way through first.
• Only use this pen for you – do not let anyone else use it.
• The numbers on the black dose selection dial and the red dose control scale are measured in
International Units or IU. Your doctor will have told you how many IU to inject each day.
• Give yourself the injection at the same time each day.
Wash your hands
• It is important that your hands and the things you use to get your pen ready are as clean as
possible.
Find a clean area
• A good place is a clean table or kitchen surface.
Get together everything you need and lay them out:
• 2 alcohol swabs
• the pre-filled pen
• a needle.
1. pencap
2. outer needle cap
3. peel-offseal
4. inner needle cap
5. removableneedle
6. threadedtip
7. liquidholder
8. plungerpiston
9. dosearrow
10. black dose selection dial (in IU FSH)
11. red dose control scale
12. grey marker of complete dose
delivery
13. injection button
Please note: The scale that can be seen through the liquid holder shows how much of the medicine is
left in the pen. Do not use it to set the dose.
Getting a new pen ready for the first time
Put on a needle
• Take a new needle – only use the “single-use” needles supplied for the GONAL-f pre-filled
pen.
• Check that the peel-off seal on the outer needle cap is not damaged or loose. If it is
damaged or loose, do not use the needle and get another. Throw away the unused needle
with the outer needle cap still on, in your household rubbish.
• Pull off the peel-off seal.
• Hold the outer needle cap firmly.
• Press the threaded tip of the pen into the outer needle cap and twist it clockwise.
• Twist it until it is firmly fixed.
Getting the liquid in the pen ready for use
(also called “priming” the pen)
• Set the dose arrow to 37.5 using the black dose selection dial - look for the small dot.
• Pull out the injection button as far as it will go.
• Take off the outer needle cap.
• Then take off the inner needle cap and hold the pen with the needle pointing upwards.
• Tap the liquid holder gently with your finger.
− this lets any air bubbles rise up towards the needle.
• With the needle still pointing upwards, press the injection button fully.
− A drop of liquid will appear at the tip of the needle; this shows that your pen is ready
for injection.
− This liquid at the needle tip is the “over-fill” from the pen.


• If no liquid appears the first time, pull out the injection button as far as it will go and press
the button again until a drop of liquid appears.
Set the dose you need by turning the black dose dial in either direction
• Turn the dial until the arrow is pointing to the dose you need.
− The black dial lets you set the dose in steps of 37.5 IU.
− The smallest dose is 37.5 IU and the largest is 450 IU.
• Important: carefully check the dose dial before moving on to the next step. This is because
the dose cannot be changed after you have pulled out the injection button.
• If you realise that you have set and loaded a wrong dose, do not inject it. Discard the wrong
dose in the sink and set the dose again.
Once you have set your dose, load the dose by pulling the injection button out as far as it
will go
• Take care to pull the button straight and not to twist it out – twisting it might change the
dose which you have set.
• When the injection button is pulled out, the loaded dose is shown on the red dose control
scale which appears. It is shown by the last mark (flat arrow).
• The example in the picture shows the injection button pulled out and a loaded dose of
150 IU. The grey marker can now be seen.
•
Important
: check the red dose control scale on the injection button to make sure that the
full dose has been loaded.
• If the loaded dose is lower than the set dose, then there was not enough medicine left in
your pen for this dose.
− If this happens, follow the instructions given at the bottom of this column in the
second bullet point of the “More information about the red dose control scale”
section.
• If the same dose is required every time, then the dose arrow can be left pointing at the same
position on the dose dial.
Choose the place to give the injection
– where your doctor or nurse has told you (e.g. tummy,
front of thigh). To minimise skin irritation, select a different injection site each day.
Clean the skin where the injection is going by wiping with an alcohol swab
Inject the dose as you were told by your doctor or nurse
• Put the needle into the skin and press the injection button as far as it will go.
• Check that the grey marker on the injection button is no longer visible.
− This confirms that the dose has been given.
− You must keep the needle in the skin
with the injection button pressed down
for at
least 10 seconds.
− After 10 seconds, keep the injection button pressed down, and take the needle out of
the skin.
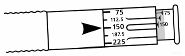

Taking off the needle
• Take off the needle after each injection.
− Hold the pen firmly by the liquid holder.
− Carefully put back the outer needle cap onto the needle.
− Then grip the outer needle cap and unscrew the needle – do this by turning anti-
clockwise.
− Throw away the used needle with outer needle cap on, in your household rubbish.
− Now put the pen cap back onto the pen.
Storing the pen
• First take off the needle and put back on the pen cap - as described above.
• Then store the pen in a safe place.
− It is best to put it back into its original package.
• When the pen is empty, throw it away in your household rubbish.
More information about the red dose control scale
• When the pen is nearly empty, there may not be enough left for your last dose from that pen. The
red dose control scale on the injection button is for you to check whether there is enough for your
last dose from the pen.
–
It can only be pulled out as far as the mark (flat arrow) showing the amount of medicine
left in the pen.
• If the loaded dose is not enough to complete your injection, you can do one of two things:
–
Either
inject the part dose – what is left in the pen. If you do this, write down straight away
how much you have injected. Then give the rest of your dose from a new pen.
–
Or
throw away the pen and inject the full dose using a new pen.

Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/gonalf.html
Copyright © 1995-2021 ITA all rights reserved.
|
















































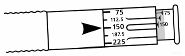


 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































