Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
Macugen 0.3 mg solution for injection
QUALITATIVE AND QUANTITATIVE COMPOSITION
A single dose pre-filled syringe delivers 1.65 mg pegaptanib sodium, corresponding to 0.3 mg of the
free acid form of the oligonucleotide, in a nominal volume of 90 microlitres.
For a full list excipients, see section 6.1.
Solution for injection (injection).
The solution is clear and colourless.
4.1 Therapeutic indications
Macugen is indicated for the treatment of neovascular (wet) age-related macular degeneration (AMD)
in adults (see section 5.1).
4.2
Posology and method of administration
Macugen should only be administered by ophthalmologists experienced in intravitreal injections.
The patient’s medical history for hypersensitivity reactions should be carefully evaluated prior to
performing the intravitreal procedure (see section 4.4)
Macugen 0.3 mg should be administered once every six weeks (9 injections per year) by intravitreal
injection into the affected eye.
Following the injection, transient increases in intraocular pressure were seen in Macugen treated
patients. Therefore, the perfusion of the optic nerve head and intraocular pressure should be
monitored. Moreover patients should be closely monitored for vitreous haemorrhage and
endophthalmitis in the two weeks following the injection. Patients should be instructed to report any
symptoms suggestive of these conditions without delay (see section 4.4).
After 2 consecutive injections of Macugen, if a patient does not demonstrate a treatment benefit (loss
of less than 15 letters of visual acuity) at the 12-week visit, consideration should be given to stopping
or withholding Macugen therapy.
Elderly
No special considerations are needed.
Hepatic impairment
Macugen has not been studied in patients with hepatic impairment.
However, no special considerations are needed in this population (see section 5.2)
Renal impairment
Macugen has not been adequately studied in patients with severe renal impairment, however dose
adjustments are not recommended in patients with mild or moderate renal impairment (see section
5.2).
Gender
No special considerations are needed.
The safety and efficacy of Macugen in children under 18 years has not yet been established. No data
are available.
For intravitreal injection use only.
Macugen should be inspected visually for particulate matter and discoloration prior to administration
(see section 6.6).
The injection procedure should be carried out under aseptic conditions, which includes the use of
surgical hand disinfection, sterile gloves, a sterile drape and a sterile eyelid speculum (or equivalent)
and the availability of sterile paracentesis (if required).
Adequate anaesthesia and a broad-spectrum
topical microbicide should be administered prior to the injection.
Hypersensitivity to the active substance or to any of the excipients.
Active or suspected ocular or periocular infection.
4.4 Special warnings and precautions for use
As expected with intravitreal injections, transient increases in intraocular pressure may be seen.
Therefore, the perfusion of the optic nerve head should be verified and elevation of intraocular
pressure should be managed appropriately post injection.
Immediate (on the day of injection) and delayed intravitreous haemorrhages may occur following
pegaptanib injections (see section 4.2).
Intravitreal injection procedures are associated with a risk of endophthalmitis; in Macugen clinical
trials, the incidence of endophthalmitis was 0.1% per injection (see section 4.2).
Cases of anaphylaxis/anaphylactoid reactions, including angioedema, have been observed within
several hours after the pegaptanib intravitreal administration procedure in the post-marketing
experience. A direct relationship to Macugen or any of the various treatments administered as part of
the injection preparation procedure, or to other factors has not been established in these cases.
4.5 Interaction with other medicinal products and other forms of interaction
Drug interaction studies have not been conducted with Macugen. Pegaptanib is metabolised by
nucleases and therefore cytochrome P450 mediated drug interactions are unlikely.
Two early clinical studies conducted in patients who received Macugen alone and in combination with
PDT (photodynamic therapy) revealed no apparent difference in the plasma pharmacokinetics of
pegaptanib.
Fertility, pregnancy and lactation
Pregnancy
Pegaptanib has not been studied in pregnant women. Animal studies are insufficient, but have shown
reproductive toxicity at high systemic exposure levels (see section 5.3). The potential risk to humans is
unknown. The systemic exposure to pegaptanib is expected to be very low after ocular administration.
Nevertheless, Macugen should be used during pregnancy only if the potential benefit to the mother
justifies the potential risk to the foetus.
Breast feeding
It is not known whether Macugen is excreted in human milk. Macugen is not recommended during
breast-feeding.
4.7 Effects on ability to drive and use machines
Patients may experience temporary visual blurring after receiving Macugen by intravitreal injection.
These after effects of the intravitreal injection may have a minor influence on the ability to drive and
use machines.
They should not drive or use machines until this has resolved
Macugen was administered to 892 patients in controlled studies for one year (total number of
injections = 7545, mean number of injections/patient = 8.5) at doses of 0.3, 1.0 and 3.0 mg. All three
doses shared a similar safety profile. In the 295 patients who were treated with the recommended dose
of 0.3 mg for one year (total number of injections = 2478, mean number of injections/patient = 8.4),
84% of the patients experienced an adverse event attributed by the investigators as being related to the
injection procedure, 3% of the patients experienced a Serious Adverse Event potentially related to the
injection procedure, and 1% experienced an adverse event potentially related to the injection
procedure that led to study treatment discontinuation. Twenty seven percent (27%) of the patients
experienced an adverse reaction. Two patients (0.7%) experienced serious adverse reactions; one of
these patients had an aortic aneurysm; the other had a retinal detachment and retinal haemorrhage,
which led to discontinuation of treatment.
Three hundred seventy four (374) patients received continuous treatment with Macugen for up to
2 years (128 at 0.3 mg, 126 at 1 mg, and 120 at 3 mg). The overall safety data were consistent with the
Year 1 safety data, and no new safety signals emerged. In the 128 patients who were treated with the
recommended dose of 0.3 mg for up to 2 years (total number of injections in second year = 913, mean
number of injections in the second year = 6.9), there was no evidence of increased in frequency of
adverse reactions compared to those seen during the first year.
Serious ocular adverse reactions reported in Macugen treated patients included endophthalmitis (12
cases, 1%), retinal haemorrhage (3 cases, < 1%), vitreous haemorrhage (2 cases, < 1%) and retinal
detachment (4 cases, < 1%).
The safety data described below summarise all procedure and adverse reactions in the 295 patients in
the 0.3 mg treatment group. The adverse reactions are listed by system organ class and frequency
(very common (≥1/10), common (≥1/100 and <1/10), and uncommon (≥1/1,000 and <1/100), not
known (cannot be estimated from the available data)).
Reports from post-marketing experience are included in italics.
MedDRA system organ class
anterior chamber inflammation, eye pain, increased
intraocular pressure, punctate keratitis, vitreous floaters and
vitreous opacities
abnormal sensation in eye, cataract, conjunctival
haemorrhage, conjunctival hyperaemia, conjunctival
oedema, conjunctivitis, corneal dystrophy, corneal
epithelium defect, corneal epithelium disorder, corneal
oedema, dry eye, endophthalmitis, eye discharge, eye
inflammation, eye irritation, eye pruritus, eye redness, eye
swelling, eyelid oedema, lacrimation increased, macular
degeneration, mydriasis, ocular discomfort, ocular
hypertension, periorbital haematoma, photophobia,
photopsia, retinal haemorrhage, vision blurred, visual acuity
reduced, visual disturbance, vitreous detachment, and
vitreous disorder
asthenopia, blepharitis, conjunctivitis allergic, corneal
deposits, eye haemorrhage, eyelids pruritus, keratitis,
vitreous haemorrhage, pupillary reflex impaired, corneal
abrasion, retinal exudates, eyelid ptosis, retinal scar,
chalazion, corneal erosion, decreased intraocular pressure,
injection site reaction, injection site vesicles, retinal
detachment, corneal disorder, retinal artery occlusion, retinal
tear, ectropion, eye movement disorder, eyelid irritation,
hyphaema, pupillary disorder, iris disorder, ocular icterus,
anterior uveitis, deposit eye, iritis, optic nerve cupping,
pupillary deformity, retinal vein occlusion, and vitreous
prolapse
Ear and labyrinth disorders
deafness, Meniere's disease aggravated, vertigo
hypertension, aortic aneurysm
Respiratory, thoracic and
mediastinal disorders
Gastrointestinal disorders


Skin and subcutaneous tissue
disorders
contact dermatitis, eczema, hair colour changes, rash,
pruritus, night sweats
Musculoskeletal and connective
tissue disorders
General disorders and
administration site conditions
fatigue, rigors, tenderness, chest pain, influenza like illness
increased gamma-glutamyltransferase activity
Injury, poisoning and procedural
complications
* Post-marketing experience:
Cases of anaphylaxis/anaphylactoid reactions, including angioedema,
have been reported in patients within several hours after administration of pegaptanib along with
various medicinal products administered as part of the injection preparation procedure (see sections
4.2
and 4.4).
Overdose with Macugen has not been reported in clinical trials and is considered unlikely as it would
require multiple injections. There is therefore no data on acute symptoms, signs or sequalae
associated with overdose.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: Ophthalmologicals, Ocular vascular disorder agents, ATC Code
S01LA03.
Mechanism of action
Pegaptanib is a pegylated modified oligonucleotide that binds with high specificity and affinity to
extracellular Vascular Endothelial Growth Factor (VEGF
165
) inhibiting its activity. VEGF is a secreted
protein that induces angiogenesis, vascular permeability and inflammation, all of which are thought to
contribute to the progression
of the neovascular (wet) form of AMD.
Pharmacodynamic effects
VEGF
165
is the VEGF isoform preferentially involved in pathological ocular neovascularisation. The
selective inhibition in animals with pegaptanib proved as effective at suppressing pathological
neovascularisation as pan-VEGF inhibition, however pegaptanib spared the normal vasculature
whereas pan-VEGF inhibition did not.
Reductions in the growth of mean total lesion size, choroidal neovascularisation (CNV size), and
fluorescein leak size, have been shown in patients with AMD treated with Macugen.

Clinical efficacy and safety
Pegaptanib was studied in two controlled, double-masked, and identically designed randomised
studies (EOP1003; EOP1004) in patients with neovascular AMD. A total of 1190 patients were treated
(892 pegaptanib, 298 sham (control)) with a median age of 77 years. Patients received a mean of
between 8.4-8.6 treatments out of possible 9 total across all treatment arms in the first year.
Patients were randomised to receive sham or 0.3 mg, 1 mg or 3 mg pegaptanib administered as
intravitreal injections every 6 weeks for 48 weeks. Verteporfin photodynamic therapy (PDT) was
permitted in patients with predominantly classic lesions at the discretion of the investigators.
The two trials enrolled patients, including all neovascular AMD lesion subtypes (25% predominantly
classic, 39% occult with no classic and 36% minimally classic), lesion sizes up to 12 disc areas, of
which up to 50% could be comprised of subretinal haemorrhage and/or up to 25% fibrotic scar or
atrophic damage. Patients had up to one prior PDT and baseline visual acuity in the study eye between
20/40 and 20/320.
At one year, pegaptanib 0.3 mg exhibited a statistically significant treatment benefit for the primary
efficacy endpoint; proportion of patients losing less than 15 letters of visual acuity (prespecified
pooled analysis, pegaptanib 0.3 mg 70% versus Sham 55%, p = 0.0001; EOP1003 pegaptanib 0.3 mg
73% versus Sham 59%, p = 0.0105; EOP1004 pegaptanib 0.3 mg 67% versus Sham 52%, p = 0.0031).
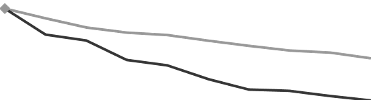
Mean Change in Visual Acuity Over Time; Year 1; ITT (LOCF)
Weeks
N: number of patients enrolled
Pegaptanib 0.3mg showed treatment benefit regardless of baseline lesion subtype, lesion size and
visual acuity as well as age, gender, iris pigmentation and prior and/or baseline PDT usage.
At the end of the first year (week 54), 1053 patients were re-randomized to either continue or
discontinue treatment through week 102.
On average, the treatment benefit was maintained at 102 weeks with continuing preservation of visual
acuity for patients re-randomized to continue pegaptanib. Patients who were re-randomized to
discontinue pegaptanib after one year, lost visual acuity during the second year.









































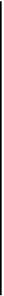
Summary of Mean Changes in Visual Acuity from Base
line to Weeks 6, 12, 54 and 102 (LOCF)
Sham-
sham/sham+
discontinued
Sham-
sham/sham+
discontinued
Mean change
in VA Week
12
Mean change
in VA Week
54
Mean change
in VA Week
102
Data over a two-year period indicate that Macugen treatment should be initiated as early as possible.
In advanced disease the initiation and continuation of Macugen therapy should consider the potential
for useful vision in the eye.
Macugen therapy administered to both eyes concurrently has not been studied.
The safety and efficacy of Macugen beyond two years has not been demonstrated.
The European Medicines Agency has waived the obligation to submit the results of studies with
Macugen in all subsets of the paediatric population in diabetic retinopathy. See section 4.2 for
information on paediatric use.
5.2
Pharmacokinetic properties
Absorption:
In animals, pegaptanib is slowly absorbed into the systemic circulation from the eye after intravitreal
administration. The rate of absorption from the eye is the rate-limiting step in the disposition of
pegaptanib in animals and is likely to be in humans. In humans, the average ± standard deviation
apparent plasma half-life of pegaptanib after a 3 mg (10-times the recommended dose) monocular
dose is 10 ± 4 days.
A mean maximum plasma concentration of about 80 ng/ml occurs within 1 to 4 days after a 3 mg
monocular dose in humans. The mean area under the plasma concentration-time curve (AUC) is about
25 g·hr/ml at this dose. Pegaptanib does not accumulate in the plasma when administered
intravitreally every 6 weeks. At doses below 0.5 mg/eye, pegaptanib plasma concentrations do not
likely exceed 10 ng/ml.
The absolute bioavailability of pegaptanib after intravitreal administration has not been assessed in
humans, but is approximately 70-100% in rabbits, dogs and monkeys.
In animals that received doses of pegaptanib up to 0.5 mg/eye to both eyes, plasma concentrations
were 0.03% to 0.15% of those in the vitreous humour.








Distribution/Biotransformation/Excretion:
In mice, rats, rabbits, dogs and monkeys, pegaptanib distributes primarily into plasma volume and is
not extensively distributed to peripheral tissues after intravenous administration. Twenty-four hours
after intravitreous administration of a radiolabeled dose of pegaptanib to both eyes of rabbits,
radioactivity was mainly distributed in vitreous humour, retina and aqueous humour. After intravitreal
and intravenous administrations of radiolabeled pegaptanib to rabbits, the highest concentrations of
radioactivity (excluding the eye for the intravitreal dose) were obtained in the kidney. In rabbits, the
component nucleotide, 2’-fluorouridine is found in plasma and urine after single radiolabeled
pegaptanib intravenous and intravitreal doses. Pegaptanib is metabolised by endo- and exonucleases.
In rabbits, pegaptanib is eliminated as parent drug and metabolites primarily in the urine.
Special populations:
Pegaptanib pharmacokinetics is similar in female and male patients and within the age range 50 to
90 years.
Pegaptanib sodium has not been adequately studied in patients with creatinine clearance below
20 ml/min. A decrease in creatinine clearance down to 20 ml/min may be associated with up to a
2.3-fold increase in pegaptanib AUC. No special considerations are needed in patients with creatinine
clearance above 20 ml/min who are treated with the recommended dose of pegaptanib sodium 0.3 mg.
Pegaptanib pharmacokinetics have not been studied in patients with hepatic impairment. The systemic
exposure is expected to be within a well tolerated range in patients with hepatic impairment, as a 10
fold higher dose (3 mg/eye) was well tolerated.
5.3 Preclinical safety data
Non-clinical data revealed no special hazard for humans based on conventional studies of safety
pharmacology, repeated dose toxicity and genotoxicity. There are no studies on the carcinogenic
potential of pegaptanib.
Pegaptanib produced no maternal toxicity and no evidence of teratogenicity or foetal mortality in mice
at intravenous doses of 1 to 40 mg/kg/day. Reduced body weight (5%) and minimal delayed
ossification in forepaw phalanges were observed, only at exposure levels based on AUC of over 300
fold greater than that expected in humans. These finding are therefore considered to be of limited
clinical relevance. In the 40 mg/kg/day group, pegaptanib concentrations in the amniotic fluid were
0.05% of the maternal plasma levels. There are no reproductive toxicity studies in rabbits.
No data are available to evaluate male or female mating or fertility indices.
PHARMACEUTICAL PARTICULARS
Sodium chloride
Monobasic sodium phosphate monohydrate
Dibasic sodium phosphate heptahydrate
Sodium hydroxide (for pH adjustment)
Hydrochloric acid (for pH adjustment)
Water for injections
In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal
products.
6.4 Special precautions for storage
Store in a refrigerator (2
o
C -8
o
C). Do not freeze.
6.5
Nature and contents of container
Macugen is supplied in a single dose pack.
Each pack contains a pouch in a carton containing a 1 ml pre-filled syringe, Type 1 glass, sealed with
an elastomeric plunger stopper and a pre-attached plunger rod, held by a plastic clip. The syringe has a
pre-attached polycarbonate plastic luer lock adaptor and the tip is sealed with an elastomeric tip cap.
The pack is supplied without a needle.
6.6 Special precautions for disposal and other handling
Macugen is for single use only. If the solution appears cloudy, particles are observed or if there is
evidence of damage to the syringe, or if the plastic clip is missing or not attached to the syringe, that
Macugen dose should not be used.
Prior to the administration, the syringe should be removed from the plastic clip and the tip cap
removed. A 27 or 30 G x ½ inch needle should be attached to the luer lock adaptor, to allow the
administration of the medicinal product.
The syringe should be checked with the needle pointing up for the presence of bubbles. If there are
bubbles, the syringe should be gently tapped with a finger until the bubbles rise to the top of the
syringe. Then, the plunger should be slowly pushed up to force the bubbles out of the syringe. The
plunger stopper should not be pulled back.
The last rib of the plunger stopper (closest to the plunger rod) should not be pushed past the dose line
printed on the syringe. Immediately prior to administration this last rib of the plunger should be
aligned with the dose line to ensure the delivery of the appropriate dose. At this point, the entire
content of the syringe should be injected.
Macugen should be stored in a refrigerator at 2ºC to 8ºC. The solution to be injected should reach
room temperature before injecting. Macugen should be discarded if kept at room temperature for more
than two weeks. To prevent contamination, the Macugen syringe should not be removed from the
pouch until the patient has been prepared for injection.
Any unused medicinal product or waste material should be disposed of in accordance with local
requirements.
MARKETING AUTHORISATION HOLDER
Pfizer Limited
Ramsgate Road
Sandwich, Kent
CT13 9NJ
United Kingdom
MARKETING AUTHORISATION NUMBER(S)
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 31/01/2006
Date of latest renewal:
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
A.
MANUFACTURING AUTHORISATION HOLDER
RESPONSIBLE FOR BATCH RELEASE
B.
CONDITIONS OF THE MARKETING AUTHORISATION
MANUFACTURING AUTHORISATION HOLDER RESPONSIBLE FOR BATCH
RELEASE
Name and address of the manufacturer responsible for batch release
Pfizer Ireland Pharmaceuticals
Pottery Road
Dun Laoghaire
Co Dublin
Ireland
CONDITIONS OF THE MARKETING AUTHORISATION
CONDITIONS OR RESTRICTIONS REGARDING SUPPLY AND USE IMPOSED ON
THE MARKETING AUTHORISATION HOLDER
Medicinal product subject to restricted medical prescription (See Annex I: Summary of Product
Characteristics, section 4.2).
CONDITIONS OR RESTRICTIONS WITH REGARD TO THE SAFE AND
EFFECTIVE USE OF THE MEDICINAL PRODUCT
The Marketing Authorisation Holder must implement nationally, prior to marketing, and as agreed
with the competent authorities in the Member States:
An educational plan for physicians and health care providers which is aimed at risk
minimisation and to support safe and effective use for the product. This plan shall consist of
measures aiming to minimise adverse events associated with the intravitreal injection
procedure (e.g. endophthalmitis) through adequate education about:
a)
The intravitreal procedure as it was performed in the pivotal clinical studies
b)
Sterile techniques to minimize risk of infection
c)
Use of antibiotics
d)
Use of povidone iodine
e)
Performing lid scrubs
f)
Use of anesthetic to ensure patient comfort
g)
Techniques for the intravitreal injection
h)
Management of intraocular pressure (IOP)
i)
Management of endophthalmitis
j)
Understanding the risk factors involved in developing endophthalmitis
k)
Reporting of serious adverse events
An educational plan for patients which is aimed at risk minimisation and to support safe and
effective use for the product. This plan shall consist of measures to provide adequate
education on:
l)
Key signs and symptoms of serious adverse events associated with the intravitreal injection
procedure
m)
When to seek urgent attention from the health care provider
Pharmacovigilance system
The MAH must ensure that the system of pharmacovigilance, as described in version 2.0 presented in
Module 1.8.1. of the Marketing Authorisation, is in place and functioning before and whilst the
product is on the market.
Risk Management Plan
The Marketing Authorisation Holder has committed to performing the studies and monitoring which
are detailed in the risk management plan, as part of the Pharmacovigilance plan.
In addition, the Marketing Authorisation Holder committed to provide a proposal for a methodology to
assess the effectiveness of risk minimisation measures across the EU, including milestones for such
assessment. This should be in line with the CHMP Guideline on Risk Management Systems for
Medicinal Products for Human use and should be submitted within 30 days after the Commission
Decision.
PSUR
The MAH will continue to submit yearly PSURs until otherwise specified by the CHMP
.
ANNEX III
LABELLING AND PACKAGE LEAFLET
PARTICULARS TO APPEAR ON THE OUTER PACKAGING
NAME OF THE MEDICINAL PRODUCT
Macugen 0.3 mg solution for injection
pegaptanib
STATEMENT OF ACTIVE SUBSTANCE(S)
A single dose pre-filled syringe delivers 1.65 mg pegaptanib sodium, corresponding to 0.3 mg of the
free acid form of the oligonucleotide, in a nominal volume of 90 microlitres.
Sodium chloride, monobasic sodium phosphate monohydrate, dibasic sodium phosphate heptahydrate,
sodium hydroxide, hydrochloric acid, water for injections.
PHARMACEUTICAL FORM AND CONTENTS
Solution for injection, 90 µl.
This pack contains one pre-filled syringe, a plunger stopper and a pre-attached plunger rod and is
supplied without a needle.
METHOD AND ROUTE(S) OF ADMINISTRATION
Read the package leaflet before use.
Intravitreal use.
SPECIAL WARNING THAT THE MEDICINAL PRODUCT MUST BE STORED OUT
OF THE REACH AND SIGHT OF CHILDREN
Keep out of the reach and sight of children.
OTHER SPECIAL WARNING(S), IF NECESSARY
SPECIAL STORAGE CONDITIONS
Store in a refrigerator. Do not freeze.






















10. SPECIAL PRECAUTIONS FOR DISPOSAL OF UNUSED MEDICINAL PRODUCTS
OR WASTE MATERIALS DERIVED FROM SUCH MEDICINAL PRODUCTS, IF
APPROPRIATE
11. NAME AND ADDRESS OF THE MARKETING AUTHORISATION HOLDER
Pfizer Ltd
Ramsgate Road
Sandwich, Kent
CT13 9NJ
United Kingdom
MARKETING AUTHORISATION NUMBER(S)
GENERAL CLASSIFICATION FOR SUPPLY
Medicinal product subject to medical prescription.
Justification for not including Braille accepted















PACKAGE LEAFLET: INFORMATION FOR THE USER
Macugen 0.3 mg solution for injection
Pegaptanib
Read all of this leaflet carefully before your treatment with Macugen begins
-
Keep this leaflet. You may need to read it again
-
If you have any further questions, please ask your doctor or pharmacist
-
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet,
please tell your doctor or pharmacist.
In this leaflet
:
1. What Macugen is and what it is used for
2. Before Macugen is used
3. How the intravitreal injection of Macugen is administered
4. Possible side effects
5.
How to store Macugen
6.
Further information
WHAT MACUGEN IS AND WHAT IT IS USED FOR
Macugen is an ophthalmic medicine which means it is for eye treatment only.
Macugen is used for the treatment of the wet form of age-related macular degeneration (AMD). This
disease leads to vision loss resulting from damage to the central part of the retina (called the macula),
at the back of the eye. The macula enables the eye to provide the fine central vision that is needed for
activities such as driving a car, reading fine print and other similar tasks.
In the wet form of AMD, abnormal blood vessels grow under the retina and macula. These new blood
vessels may bleed and leak fluid, causing the macula to bulge or lift up, thus distorting or destroying
central vision. Under these circumstances vision loss may be rapid and severe. Macugen works by
inhibiting the growth of these abnormal blood vessels and by stemming the bleeding and leakage.
Macugen is used for the treatment of all types of abnormal blood vessels growth in adult AMD
patients.
Macugen must not be used
If you are hypersensitive (allergic) to pegaptanib or any of the other ingredients of Macugen.
If you have an infection in or around the eye.
Take special care with Macugen
Macugen is given as an injection into the eye. Occasionally, an infection or bleeding in the eye can
occur after Macugen treatment (in the next two weeks). It is important to identify and treat these types
of conditions as soon as possible. Please tell your doctor immediately if you notice any of the
following symptoms: eye pain or increased discomfort, worsening eye redness, blurred or decreased
vision, increased sensitivity to light, increased number of small particles in your vision.
If your doctor
cannot be reached for any reason, an alternate should be contacted immediately.
In some patients the pressure inside the treated eye may increase for a short period directly after the
injection. Your doctor may monitor this after each injection.
Children
Macugen should not be used in children and adolescents under 18 years old.
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines
obtained without a prescription.
Pregnancy
There is no experience of using Macugen in pregnant women; therefore the potential risks are
unknown. If you are pregnant or planning to become pregnant, please discuss this with your doctor
before Macugen treatment.
Breast-feeding
It is not known whether Macugen is excreted in human milk. Macugen is not recommended during
breast-feeding. Ask your doctor or pharmacist for advice before Macugen treatment.
Driving and using machines
You may experience temporary visual blurring after receiving Macugen. If you are affected, do not
drive or use machines until this resolves.
Important information about some of the ingredients of Macugen
This medicine contains less than 1 mmol sodium (23 mg) per 90 microlitre dose, i.e. essentially
‘sodium-free’.
HOW THE INTRAVITREAL INJECTION OF MACUGEN IS ADMINISTERED
All injections of Macugen will be administered by your doctor.
Macugen is administered as a single injection (0.3 mg) into your eye at intervals of 6 weeks (i.e.
9 times per year). The injection is given into the vitreous of the eye, which is the jelly-like substance
inside the eye. Your doctor will monitor your condition and recommend how long you should be
treated with Macugen.
Before the treatment is given your doctor may ask you to use antibiotic eye drops, or to wash your
eyes carefully. Please tell your doctor if you are known to be allergic to any substance. Please follow
these instructions carefully.
Before the injection, your doctor will give you some local anaesthetic (numbing medicine). This will
reduce or prevent any pain you might have with the injection, which is a simple and rapid procedure.
After each injection you might be asked to use antibiotic eye drops (or another type of antibiotic
treatment) to guard against eye infection.
If you forget to attend an appointment
Contact the hospital or clinic as soon as possible to re-schedule your appointment.
If you have any further questions on the use of this medicine, ask your doctor of pharmacist.
Like all medicines, Macugen can cause side effects although not everybody gets them.
In some rare cases, serious allergic reaction has been reported soon after the injection. Please seek
immediate medical help if you experience any of the following soon after the injection: sudden onset
of breathing difficulty or wheezing, swollen mouth, face, hands or feet, itching skin, fainting, rapid
pulse, stomach cramps, nausea, vomiting or diarrhoea.
Uncommonly, an infection in the internal portion of the eye can occur after Macugen treatment in the
next two weeks. The symptoms you might experience are described in section 2 of this leaflet ("Take
special care with Macugen"). Please read section 2. It tells you what to do if you have any of these
symptoms.
The frequency of possible side effects listed below is defined using the following convention:
very common (affects more than 1 user in 10)
common (affects 1 to 10 users in 100)
uncommon (affects 1 to 10 users in 1,000)
rare (affects 1 to 10 users in 10,000)
very rare (affects less than 1 user in 10,000)
Very common side effects are most probably caused by the injection procedure rather than the
medicine, and include: eye inflammation, eye pain, increased pressure inside the eye, small marks on
the eye surface (punctate keratitis), small particles or spots in your vision (vitreous floaters or
opacities).
Other common eye side effects reported to be possibly caused by the medicine or by the injection
procedure include: blurred vision, visual disturbance, eye discomfort, decreased vision, increased
sensitivity to light, appearance of flashing lights, bleeding that occurs around the eye (periorbital
bleeding), bloodshot eye (conjunctival haemorrhage), disorder of the jelly portion inside the eye
(vitreous disorder), such as displacement or tear (vitreous detachment), clouding of the lens (cataract),
disorder of the surface of the eye (cornea), , swelling or inflammation of the eyelid, swelling of the
area on the inside of the eyelid or the outer surface of the eye (conjunctiva), eye inflammation, tears,
inflammation of the conjunctiva (conjunctivitis), dryness, eye discharge, eye irritation, itching of the
eye, eye redness or enlargement of the pupil,
Other common non-visual side effects reported to be possibly caused by the medicine or by the
injection procedure includes: headache or nasal discharge.
Uncommon eye side effects reported to be possibly caused by the drug or by the injection procedure
include: inflammation of your eye or of the outer surface of the eye, bleeding in the eye or the internal
portion of the eye (vitreous), eye strain, inflammation of the central part of the surface of the eye
(keratitis), small deposits on the eye or on the surface of the eye (cornea), deposits in the back of the
eye, itching of the eyelids, disturbance in your eye’s reaction to the light (pupillary reflex impaired),
small erosion on the central part of the surface of the eye (cornea), drooping eyelid, scar inside the eye
(retinal scar), small lump on your eyelid due to inflammation (chalazion), decreased pressure inside the
eye, injection site reaction, injection site vesicles, displacement or tear of a layer in the back of the eye
(retina), disorder of the pupil, of the coloured part of the eye (iris), retinal artery occlusion, eversion of
the eyelid, eye movement disorder, eyelid irritation, blood in your eye, discoloured eye, deposit eye,
inflammation of the eye (iritis), optic nerve cupping, deformation of the pupil, occlusion of the vein at
the back of the eye, discharge of inner jelly of the eye.
Uncommon non-visual side effects reported to be possibly caused by the drug or by the injection
procedure include: nightmare, depression, deafness, vertigo, palpitations, high blood pressure,
dilatation of the aorta (the main blood vessel), inflammation of the higher respiratory tract, vomiting,
indigestion, irritation and inflammation of the skin, hair colour changes, rash, itching, night sweats,
back pain, tiredness, shivering, tenderness, chest pain, sudden fever, generalised aches and pains,
elevation of the liver enzymes, abrasion.
If you notice other side effects not mentioned in this leaflet, please inform your doctor or pharmacist.
Keep out of the reach and sight of children.
Do not use after the expiry date
stated which is on the label and carton after EXP. The expiry date
refers to the last day of that month.
Store in a refrigerator (2
o
C -8
o
C).
Do not freeze.
Macugen should be discarded if kept at room temperature for more than two weeks.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to
dispose of medicines no longer required. These measures will help to protect the environment.
-
The active substance is pegaptanib. Each single dose pre-filled syringe delivers a dose of 0.3 mg
pegaptanib.
-
The other ingredients are sodium chloride, monobasic sodium phosphate monohydrate,
dibasic
sodium phosphate heptahydrate, sodium hydroxide, hydrochloric acid and water for injections.
What MACUGEN looks like and contents of the pack
Macugen solution for injection is supplied in a single dose pack.
Each pack contains a pouch in a carton, containing a 1 ml pre-filled syringe, Type I glass, sealed with
an elastomeric plunger stopper and a pre-attached plunger rod, held by a plastic clip. The syringe has a
pre-attached polycarbonate plastic .luer lock adaptor and the tip is sealed with an elastomeric tip cap.
The pack is supplied without a needle. The pre-filled syringe will be used once and then thrown away.
Marketing Authorisation Holder
Pfizer Limited
Ramsgate Road
Sandwich
CT13 9NJ
United Kingdom
Manufacturer
Pfizer Ireland Pharmaceuticals
Pottery Road
Dun Laoghaire
Co Dublin
Ireland
For any information about this medicine, please contact the local representative of the Marketing
Authorisation Holder:
België/Belgique/Belgien
Pfizer S.A. / N.V.
Tél/Tel: +32 (0)2 554 62 11
Luxembourg/Luxemburg
Pfizer S.A.
Tél/Tel: +32 (0)2 554 62 11
България
Пфайзер Люксембург САРЛ, Клон
България
Тел.: +359 2 970 4333
Magyarország
Pfizer Kft.
Tel. + 36 1 488 37 00
Česká republika
Pfizer s.r.o.
Tel: +420 283 004 111
Malta
V.J. Salomone Pharma Ltd.
Tel: + 356 21 22 01 74
Danmark
Pfizer ApS
Tlf: +45 44 20 11 00
Nederland
Pfizer bv
Tel: +31 (0)10 406 43 01
Deutschland
Pfizer Pharma GmbH
Tel: +49 (0) 30 550055 51000
Norge
Pfizer AS
Tlf: +47 67 52 61 00
Eesti
Pfizer Luxembourg SARL, Eesti filiaal
Tel: +372 6 405 328
Österreich
Pfizer Corporation Austria Ges.m.b.H.
Tel: +43 (0)1 521 15-0
Ελλάδα
Pfizer Hellas A.E.
Τλ: +30 210 678 5800
Polska
Pfizer Polska Sp. z o.o.
Tel.: + 48 22 335 61 00
España
Pfizer S.A.
Tel: +34 91 490 99 00
Portugal
Laboratórios Pfizer, Lda.
Tel: +351 21 423 5500
France
Pfizer
Tél: +33 (0)1 58 07 34 40
România
Pfizer Romania S.R.L.
Tel: +40 (0)21 207 2800
Ireland
Pfizer Healthcare Ireland
Tel: 1800 633 363 (toll free)
Slovenija
Pfizer Luxembourg SARL, Pfizer podružnica za
svetovanje s področja farmacevtske dejavnosti,
Ljubljana
Tel: + 386 (0)1 52 11 400
Ísland
Vistor hf
Sími: +354 535 7000
Slovenská republika
Pfizer Luxembourg SARL, organizačná zložka
Tel: +421-2-3355 5500
Italia
Pfizer Italia S.r.l.
Tel: +39 06 33 18 21
Suomi/Finland
Pfizer Oy
Puh./Tel: +358 (0)9 43 00 40
Κύπρος
GEO. PAVLIDES & ARAOUZOS LTD
Τηλ: +35722818087
Sverige
Pfizer AB
Tel: +46 (0)8 550 520 00
Latvija
Pfizer Luxembourg SARL, filiāle Latvijā
Tel: +371 670 35 775
United Kingdom
Pfizer Limited
Tel: +44 (0)1304 616161
Lietuva
Pfizer Luxembourg SARL, filialas Lietuvoje
Tel. +3705 2514000
This leaflet was last approved in
Detailed information on this medicine is available on the European Medicines Agency web site:
Annex IV
Grounds for one additional renewal
Grounds for one additional renewal
Based upon the data that have become available since the granting of the Marketing Authorisation,
the CHMP considers that the benefit-risk balance of Macugen remains positive, but considers that
its safety profile is to be closely monitored. The reason for this is that the issue of hypersensitivity
reactions needs to be further investigated. In addition, the CHMP considers that there is a need for
continued monitoring of potentially serious adverse ocular events and recommended that the MAH
should continue to submit yearly PSURs.
Therefore, based on the safety profile of Macugen, which requires the submission of yearly PSURs,
the CHMP concluded that the MAH should submit one additional renewal application in 5 years
time.
Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/macugen.html
Copyright © 1995-2021 ITA all rights reserved.
|


























































































































 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































