Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
Possia 90 mg film-coated tablets
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each film-coated tablet contains 90 mg ticagrelor.
For a full list of excipients, see section 6.1.
Film-coated tablet (tablet).
Round, biconvex, yellow tablets marked with ‘90’ above ‘T’ on one side and plain on the other.
4.1 Therapeutic indications
Possia, co-administered with acetylsalicylic acid (ASA), is indicated for the prevention of
atherothrombotic events in adult patients with Acute Coronary Syndromes (unstable angina, non ST
elevation Myocardial Infarction [NSTEMI] or ST elevation Myocardial Infarction [STEMI]);
including patients managed medically, and those who are managed with percutaneous coronary
intervention (PCI) or coronary artery by-pass grafting (CABG).
For further information, please refer to section 5.1.
4.2 Posology and method of administration
Posology
Possia treatment should be initiated with a single 180 mg loading dose (two tablets of 90 mg) and then
continued at 90 mg twice daily.
Patients taking Possia should also take ASA daily, unless specifically contraindicated. Following an
initial dose of ASA, Possia should be used with a maintenance dose of ASA of 75-150 mg (see
section 5.1).
Treatment is recommended for up to 12 months unless discontinuation of Possia is clinically indicated
(see section 5.1). Experience beyond 12 months is limited.
In patients with Acute Coronary Syndromes (ACS), premature discontinuation with any antiplatelet
therapy, including Possia, could result in an increased risk of cardiovascular death, or myocardial
infarction due to the patient’s underlying disease (see section 4.4). Therefore, premature
discontinuation of treatment should be avoided.
Lapses in therapy should also be avoided. A patient who misses a dose of Possia should take only one
90 mg tablet (their next dose) at its scheduled time.
Patients treated with clopidogrel can be directly switched to Possia if needed (see section 5.1).
Switching from prasugrel to Possia has not been investigated.
Elderly population
No dose adjustment is required in elderly (see section 5.2).
Renal impairment
No dose adjustment is necessary for patients with renal impairment (see section 5.2). No information
is available concerning treatment of patients on renal dialysis and therefore Possia is not recommended
in these patients.
Hepatic impairment
No dose adjustment is necessary for patients with mild hepatic impairment. Possia has not been
studied in patients with moderate or severe hepatic impairment. Its use in patients with moderate to
severe hepatic impairment is therefore contraindicated (see section 4.3, 4.4 and 5.2).
Paediatric population
The safety and efficacy of Possia in children below the age of 18 in the approved adult indication has
not been established. No data are available (see section 5.1 and 5.2).
Method of administration
For oral use. Possia can be administered with or without food.
• Hypersensitivity to the active substance or to any of the excipients.
• Active pathological bleeding
• History of intracranial haemorrhage (see section 4.8)
• Moderate to severe hepatic impairment (see section 4.3, 4.4 and 5.2)
• Co-administration of ticagrelor with strong CYP3A4 inhibitors (e.g., ketoconazole,
clarithromycin, nefazodone, ritonavir, and atazanavir) is contraindicated, as co-administration
may lead to a substantial increase in exposure to ticagrelor (see section 4.4 and 4.5).
4.4 Special warnings and precautions for use
Bleeding risk
In the phase 3 pivotal trial (PLATO [PLATelet Inhibition and Patient Outcomes], 18,624 patients) key
exclusion criteria included an increased risk for bleeding, clinically important thrombocytopenia or
anaemia, previous intracranial bleed, gastrointestinal bleed within the past 6 months or major surgery
within the past 30 days. Patients with acute coronary syndromes treated with Possia and ASA showed
an increased risk of non-CABG major bleeding and also more generally in bleeds requiring medical
attention i.e. Major + Minor PLATO bleeds, but not Fatal or Life-threatening bleeds (see section 4.8).
Therefore, the use of Possia in patients at known increased risk for bleeding should be balanced
against the benefit in terms of prevention of atherothrombotic events. If clinically indicated, Possia
should be used with caution in the following patient groups:
• Patients with a propensity to bleed (e.g. due to recent trauma, recent surgery, coagulation
disorders, active or recent gastrointestinal bleeding). The use of Possia is contraindicated in
patients with active pathological bleeding, in those with a history of intracranial haemorrhage,
and in patients with moderate to severe hepatic impairment (see section 4.3).
• Patients with concomitant administration of medicinal products that may increase the risk of
bleeding (e.g. non-steroidal anti-inflammatory drugs (NSAIDs), oral anticoagulants and/or
fibrinolytics) within 24 hours of Possia dosing.
No data exist with Possia regarding a haemostatic benefit of platelet transfusions; circulating Possia
may inhibit transfused platelets. Since co-administration of Possia with desmopressin did not decrease
template-bleeding time, desmopressin is unlikely to be effective in managing clinical bleeding events
(see section 4.5).
Antifibrinolytic therapy (aminocaproic acid or tranexamic acid) and/or recombinant factor VIIa may
increase haemostasis. Possia may be resumed after the cause of bleeding has been identified and
controlled.
Surgery
Patients should be advised to inform physicians and dentists that they are taking Possia before any
surgery is scheduled and before any new medicinal product is taken.
In PLATO patients undergoing coronary artery bypass grafting (CABG), Possia had more bleeding
than clopidogrel when stopped within 1 day prior to surgery but a similar rate of major bleeds
compared to clopidogrel after stopping therapy 2 or more days before surgery (see section 4.8). If a
patient is to undergo elective surgery and antiplatelet effect is not desired, Possia should be
discontinued 7 days prior to surgery (see section 5.1).
Patients at risk for bradycardic events
Due to observations of mostly asymptomatic ventricular pauses in an earlier clinical study, patients
with an increased risk of bradycardic events (e.g. patients without a pacemaker who have sick sinus
syndrome, 2nd or 3rd degree AV block or bradycardic-related syncope) were excluded from the main
PLATO study evaluating the safety and efficacy of Possia. Therefore, due to the limited clinical
experience, Possia should be used with caution in these patients (see section 5.1).
In addition, caution should be exercised when administering Possia concomitantly with medicinal
products known to induce bradycardia. However no evidence of clinically significant adverse
reactions was observed in the PLATO trial after concomitant administration with one or more
medicinal products known to induce bradycardia (e.g., 96% beta blockers, 33% calcium channel
blockers diltiazem and verapamil, and 4% digoxin) (see section 4.5).
During the Holter substudy in PLATO, more patients had ventricular pauses
>
3 seconds with
ticagrelor than with clopidogrel during the acute phase of their ACS. The increase in Holter-detected
ventricular pauses with ticagrelor was higher in patients with chronic heart failure (CHF) than in the
overall study population during the acute phase of ACS, but not at one month with ticagrelor or
compared to clopidogrel. There were no adverse clinical consequences associated with this imbalance
(including syncope or pacemaker insertion) in this patient population (see section 5.1).
Dyspnoea
Dyspnoea was reported by 13.8% of patients treated with Possia and by 7.8% of patients treated with
clopidogrel. In 2.2% of patients, investigators considered the dyspnoea causally related to treatment
with Possia.
It is usually mild to moderate in intensity and often resolves without need for treatment
discontinuation. Patients with asthma/COPD may have an increased absolute risk of experiencing
dyspnoea with Possia (see section 4.8). Ticagrelor should be used with caution in patients with history
of asthma and/or COPD. The mechanism has not been elucidated. If a patient reports new, prolonged
or worsened dyspnoea this should be investigated fully and if not tolerated, treatment with Possia
should be stopped.
Creatinine elevations
Creatinine levels may increase during treatment with Possia (see section 4.8). The mechanism has not
been elucidated. Renal function should be checked after one month and thereafter according to routine
medical practice, paying special attention
to patients ≥ 75 years, patients with moderate/severe renal
impairment and those receiving concomitant treatment with an ARB.
Uric acid increase
In PLATO study, patients on ticagrelor had a higher risk of hyperuricaemia than those patients
receiving clopidogrel (see section 4.8). Caution should be exercised when administering ticagrelor to
patients with history of hyperuricaemia or gouty arthritis. As a precautionary measure, the use of
ticagrelor in patients with uric acid nephropathy is discouraged.
Other
Based on a relationship observed in PLATO between maintenance ASA dose and relative efficacy of
ticagrelor compared to clopidogrel, co-administration of Possia and high maintenance dose ASA
(>300 mg) is not recommended (see section 5.1).
Co-administration of Possia with strong CYP3A4 inhibitors (e.g., ketoconazole, clarithromycin,
nefazodone, ritonavir, and atazanavir) is contraindicated (see section 4.3 and 4.5). Co-administration
may lead to a substantial
increase in Possia exposure (see section 4.5).
Co-administration of ticagrelor with strong CYP3A4 inducers (e.g. rifampicin, dexamethasone,
phenytoin, carbamazepine and phenobarbital) is discouraged, as co-administration may lead to a
decrease in exposure and efficacy of ticagrelor (see section 4.5).
Co-administration of Possia and CYP3A4 substrates with narrow therapeutic indices (i.e., cisapride
and ergot alkaloids)
is not recommended, as ticagrelor may increase the exposure to these medicinal
products (see section 4.5). The concomitant use of Possia with doses of simvastatin or lovastatin
greater than 40 mg is not recommended (see section 4.5).
Close clinical and laboratory monitoring is recommended when giving digoxin concomitantly with
Possia (see section 4.5).
No data are available on concomitant use of Possia with potent P-glycoprotein (P-gp) inhibitors (e.g.
verapamil, quinidine, cyclosporin) that may increase ticagrelor exposure. If the association cannot be
avoided, their concomitant use should be made with caution (see section 4.5).
4.5 Interaction with other medicinal products and other forms of interaction
Ticagrelor is primarily a CYP3A4 substrate and a mild inhibitor of CYP3A4. Ticagrelor is also a P-gp
substrate and a weak P-gp inhibitor and may increase the exposure of P-gp substrates.
Effects of other medicinal products on Possia
Medicinal products metabolised by CYP3A4
CYP3A4 inhibitors
• Strong CYP3A4 inhibitors – Co-administration of ketoconazole with ticagrelor increased the
ticagrelor C
max
and AUC equal to 2.4-fold and 7.3-fold, respectively. The C
max
and AUC of the
active metabolite were reduced by 89% and 56%, respectively. Other strong inhibitors of
CYP3A4 (clarithromycin, nefazodone, ritonavir, and atazanavir) would be expected to have
similar effects and their concomitant use with Possia is contraindicated (see section 4.3 and 4.4).
• Moderate CYP3A4 inhibitors – Co-administration of diltiazem with ticagrelor increased the
ticagrelor C
max
by 69% and AUC to 2.7 fold and decreased the active metabolite C
max
by 38%
and AUC was unchanged. There was no effect of ticagrelor on diltiazem plasma levels. Other
moderate CYP3A4 inhibitors (e.g. amprenavir, aprepitant, erythromycin and fluconazole) would
be expected to have a similar effect and can as well be co-administered with Possia.
CYP3A inducers
Co-administration of rifampicin with ticagrelor decreased ticagrelor C
max
and AUC by 73% and
86%, respectively. The C
max
of the active metabolite was unchanged and the AUC was decreased by
46%, respectively. Other CYP3A inducers (e.g. dexamethasone, phenytoin, carbamazepine and
phenobarbital) would be expected to decrease the exposure to Possia as well. Co-administration of
ticagrelor with potent CYP3A inducers may decrease exposure and efficacy of ticagrelor (see
section 4.4).
Clinical pharmacology interaction studies showed that co-administration of ticagrelor with heparin,
enoxaparin and ASA or desmopressin did not have any effect on the pharmacokinetics of ticagrelor or
the active metabolite or on ADP-induced platelet aggregation compared with ticagrelor alone. If
clinically indicated, medicinal products that alter haemostasis should be used with caution in
combination with Possia (see section 4.4).
No data are available on concomitant use of Possia with potent P-gp inhibitors (e.g. verapamil,
quinidine, cyclosporin) that may increase ticagrelor exposure. If clinically indicated, their concomitant
use should be made with caution (see section 4.4).
Effects of Possia on other medicinal products
Medicinal products metabolised by CYP3A4
•
Simvastatin
– Co-administration of ticagrelor with simvastatin increased simvastatin C
max
by
81% and AUC by 56% and increased simvastatin acid C
max
by 64% and AUC by 52% with
some individual increases equal to 2 to 3 fold. Co-administration of ticagrelor with doses of
simvastatin exceeding 40 mg daily could cause adverse effects of simvastatin and should be
weighed against potential benefits. There was no effect of simvastatin on ticagrelor plasma
levels. Possia may have similar effect on lovastatin. The concomitant use of Possia with doses
of simvastatin or lovastatin greater than 40 mg is not recommended (see section 4.4).
•
Atorvastatin
- Co-administration of atorvastatin and ticagrelor increased atorvastatin acid C
max
by 23% and AUC by 36%. Similar increases in AUC and C
max
were observed for all atorvastatin
acid metabolites. These increases are not considered clinically significant.
• A similar effect on other statins metabolised by CYP3A4 cannot be excluded. Patients in
PLATO receiving ticagrelor took a variety of statins, with no concern of an association with
statin safety among the 93% of the PLATO cohort taking these medicinal products.
Ticagrelor is a mild CYP3A4 inhibitor. Co-administration of Possia and CYP3A4 substrates with
narrow therapeutic indices (i.e., cisapride or
ergot alkaloids) is not recommended, as ticagrelor may
increase the exposure to these medicinal products (see section 4.4).
Medicinal products metabolised by CYP2C9
Co-administration of Possia with tolbutamide resulted in no change in the plasma levels of either
medicinal product, which suggest that ticagrelor is not a CYP2C9 inhibitor and unlikely to alter the
CYP2C9 mediated metabolism of medicinal products like warfarin and tolbutamide.
Oral contraceptives
Co-administration of Possia and levonorgestrel and ethinyl estradiol increased ethinyl estradiol
exposure approximately 20% but did not alter the pharmacokinetics of levonorgestrel. No clinically
relevant effect on oral contraceptive efficacy is expected when levonorgestrel and ethinyl estradiol are
co-administered with Possia.
P-glycoprotein (P-gp) substrates (including digoxin, cyclosporin)
Concomitant administration of Possia increased the digoxin C
max
by 75% and AUC by 28%. The mean
trough digoxin levels were increased about 30% with ticagrelor co-administration with some
individual maximum increases to 2 fold. In the presence of digoxin, the C
max
and AUC of ticagrelor
and its active metabolite were not affected. Therefore, appropriate clinical and/or laboratory
monitoring is recommended when giving narrow therapeutic index P-gp dependent medicinal products
like digoxin or cyclosporin concomitantly with Possia (see section 4.4).
Other concomitant therapy
Medicinal products known to induce bradycardia
Due to observations of mostly asymptomatic ventricular pauses and bradycardia, caution should be
exercised when administering Possia concomitantly with medicinal products known to induce
bradycardia (see section 4.4). However no evidence of clinically significant adverse reactions was
observed in the PLATO trial after concomitant administration with one or more medicinal products
known to induce bradycardia (e.g., 96% beta blockers, 33% calcium channel blockers diltiazem and
verapamil, and 4% digoxin).
In the PLATO study, Possia was commonly administered with ASA, proton pump inhibitors, statins,
beta-blockers, angiotensin converting enzyme inhibitors and angiotensin receptor blockers as needed
for concomitant conditions for long-term and also heparin, low molecular weight heparin and
intravenous GpIIb/IIIa inhibitors for short durations (see section 5.1). No evidence of clinically
significant adverse interactions with these medicinal products was observed.
Co-administration of Possia with heparin, enoxaparin or desmopressin had no effect on activated
partial thromboplastin time (aPTT), activated coagulation time (ACT) or factor Xa assays. However,
due to potential pharmacodynamic interactions, caution should be exercised with the concomitant
administration of Possia with medicinal products known to alter haemostasis (see section 4.4).
Due to reports of cutaneous bleeding abnormalities with SSRIs (e.g., paroxetine, sertraline and
citalopram), caution is advised when administering SSRIs with Possia as this may increase the risk of
bleeding.
4.6 Fertility, pregnancy and lactation
Women of childbearing potential
Women of childbearing potential should use appropriate contraceptive measures to avoid pregnancy
during Possia therapy.
Pregnancy
There are no or limited amount of data from the use of ticagrelor in pregnant women. Studies in
animals have shown reproductive toxicity (see section 5.3). Possia is not recommended during
pregnancy.
Breastfeeding
Available pharmacodynamic/toxicological data in animals have shown excretion of ticagrelor and its
active metabolites in milk (see section 5.3). A risk to newborns/infants cannot be excluded. A decision
must be made whether to discontinue breastfeeding or to discontinue/abstain from Possia therapy
taking into account the benefit of breastfeeding for the child and the benefit of therapy for the woman.
Fertility
Ticagrelor had no effect on male or female fertility in animals (see section 5.3).
4.7 Effects on ability to drive and use machines
No studies on the effects of Possia on the ability to drive and use machines have been performed.
Possia has no or negligible influence on the ability to drive and use machines.
Summary of safety profile
The safety of Possia in patients with acute coronary syndromes (UA, NSTEMI and STEMI) was
evaluated in the pivotal large phase 3 PLATO ([
PLAT
elet Inhibition and Patient
Ou
tcomes] study,
18,624 patients), which compared patients treated with Possia (loading dose of 180 mg of Possia and a
maintenance dose of 90 mg twice daily) to patients treated with clopidogrel (300-600 mg loading dose
followed by 75 mg once daily maintenance dose) both given in combination with acetylsalicylic acid
(ASA) and other standard therapies.
The most commonly reported adverse reactions in patients treated with ticagrelor were dyspnoea,
contusion and epistaxis and these reactions occurred at higher rates than in the clopidogrel treatment
group.
Tabulated summary of adverse reactions
The following adverse reactions have been identified following studies with Possia (Table 1).
Adverse reactions are classified according to frequency and System Organ Class. Frequency
categories are defined according to the following conventions: Very common (≥1/10), Common
(≥1/100 to <1/10), Uncommon (≥1/1,000 to <1/100), Rare (≥1/10,000 to <1/1,000), Very
rare (<1/10,000), Not known (cannot be estimated from the available date).
Table 1 Adverse reactions by frequency and System Organ Class (SOC)
System Organ Class
Metabolism and
nutrition disorders
Intracranial
haemorrhage
b
,
Dizziness, Headache
Eye haemorrhage
(intraocular,
conjunctival, retinal)
Ear and labyrinth
disorders
Respiratory, thoracic
and mediastinal
disorders
Gastrointestinal
disorders
Gastrointestinal
haemorrhage
d
Haematemesis,
Gastroinstestinal ulcer
haemorrhage
e
,
Haemorrhoidal
haemorrhage, Gastritis,
Oral haemorrhage
(including gingival
bleeding), Vomiting,
Diarrhoea, Abdominal
pain, Nausea,
Dyspepsia
Retroperitoneal
haemorrhage,
Constipation
Skin and subcutaneous
tissue disorders
Subcutaneous or
dermal bleeding
f
,
Bruising
g
Musculoskeletal and
connective tissue
disorders
Renal and urinary
disorders
Haemorrhage urinary
tract
h
Reproductive system
and breast disorders
Vaginal bleeding
(including
metrorrhagia)
Blood creatinine
increased
Injury, poisoning and
procedural
complications
Procedural site
haemorrhage
i
Post procedural
haemorrhage,
Haemorrhage
Wound haemorrhage,
Traumatic haemorrhage
Multiple related adverse reaction terms have been grouped together in the table and include medical terms as
described below:
Hyperuricaemia, Blood uric acid increased



















b
Cerebral haemorrhage, Haemorrhage intracranial, Haemorrhagic stroke,
c
Dyspnoea, Dyspnoea exertional, Dyspnoea at rest, Nocturnal dyspnoea
d
Gastrointestinal haemorrhage, Rectal haemorrhage, Intestinal haemorrhage, Melaena, Occult blood
e
Gastrointestinal ulcer haemorrhage, Gastric ulcer haemorrhage, Duodenal ulcer haemorrhage, Peptic ulcer
haemorrhage
f
Subcutaneous haematoma, Skin haemorrhage, Haemorrhage subcutaneous, Petechiae
g
Contusion, Haematoma, Ecchymosis, Increased tendency to bruise, Traumatic haematoma
h
Haematuria, Blood urine present, Haemorrhage urinary tract
Vessel puncture site haemorrhage, Vessel puncture site haematoma, Injection site haemorrhage, Puncture
site haemorrhage, Catheter site haemorrhage
There were no reported ADRs of haemarthrosis reported in the ticagrelor arm (n=9235) of the PLATO
study, the frequency has been calculated using the upper limit of the 95% confidence interval for the point
estimate (based on 3/X, where X represents the total sample size e.g. 9235). This is calculated as
3/9235 which equates to a frequency category of ‘rare’
Description of selected adverse reactions
Bleeding
Overall outcome of bleeding rates in the PLATO study are shown in Table 2.
Table 2 –Kaplan-Meier estimate of bleeding rates by treatment
Clopidogrel
(%/year)
N=9186
PLATO Major Fatal/Life-Threatening
Non-Procedural PLATO Major
PLATO Total Major + Minor
Non-Procedural PLATO Major + Minor
TIMI-defined Major + Minor
Bleeding category definitions:
Major Fatal/Life-threatening Bleed:
Clinically apparent with >50 g/l decrease in haemoglobin or ≥4 red cell units transfused;
or
fatal;
or
intracranial;
or
intrapericardial with cardiac tamponade;
or
with hypovolaemic shock or severe hypotension requiring pressors or surgery.
Major Other:
Clinically apparent with 30-50 g/l decrease in haemoglobin or 2-3 red cell units transfused;
or
significantly disabling.
Minor Bleed:
Requires medical intervention to stop or treat bleeding.
TIMI Major Bleed:
Clinically apparent with >50 g/l decrease in haemoglobin
or
intracranial haemorrhage.
TIMI Minor Bleed:
Clinically apparent with 30-50 g/l decrease in haemoglobin.
Possia and clopidogrel did not differ in rates of PLATO Major Fatal/Life-threatening bleeding,
PLATO total Major bleeding, TIMI Major bleeding, or TIMI Minor bleeding (Table 2). However,
more PLATO combined Major + Minor bleeding occurred with ticagrelor compared with clopidogrel.
Few patients in PLATO had fatal bleeds: 20 (0.2%) for ticagrelor and 23 (0.3%) for clopidogrel (see
section 4.4).
Age, sex, weight, race, geographic region, concurrent conditions, concomitant therapy, and medical
history, including a previous stroke or transient ischaemic attack, all did not predict either overall or
non-procedural PLATO Major bleeding. Thus no particular group was identified at risk for any subset
of bleeding.
CABG-related bleeding:
In PLATO, 42% of the 1584 patients (12% of cohort) who underwent
coronary artery bypass graft (CABG) surgery had a PLATO Major Fatal/Life-threatening bleeding
with no difference between treatment groups. Fatal CABG bleeding occurred in 6 patients in each
treatment group (see section 4.4).













Non-CABG related bleeding and non-procedural related bleeding:
Possia and clopidogrel did not
differ in non-CABG PLATO-defined Major Fatal/Life-threatening bleeding, but PLATO-defined
Total Major, TIMI Major, and TIMI Major + Minor bleeding were more common with ticagrelor.
Similarly, when removing all procedure related bleeds, more bleeding occurred with ticagrelor than
with clopidogrel (Table 2). Discontinuation of treatment due to non-procedural bleeding was more
common for ticagrelor (2.9%) than for clopidogrel (1.2%; p<0.001).
Intracranial bleeding:
There were more intracranial non-procedural bleeds with ticagrelor
(n=27 bleeds in 26 patients, 0.3%) than with clopidogrel (n=14 bleeds, 0.2%), of which 11 bleeds
with ticagrelor and 1 with clopidogrel were fatal. There was no difference in overall fatal bleeds.
Dyspnoea
Dyspnoea, a sensation of breathlessness, is reported by patients treated with Possia. Dyspnoea adverse
reactions (ADRs) (dyspnoea, dyspnoea at rest, dyspnoea exertional, dyspnoea paroxysmal nocturnal
and nocturnal dyspnoea), when combined, was reported by 13.8% of patients treated with ticagrelor
and by 7.8% of patients treated with clopidogrel. In 2.2% of patients taking ticagrelor and
by
0.6% taking clopidogrel investigators considered the dyspnoea causally related to treatment in the
PLATO study and few were serious (0.14% ticagrelor; 0.02% clopidogrel), (see section 4.4). Most
reported symptoms of dyspnoea were mild to moderate in intensity, and most were reported as a single
episode early after starting treatment.
Compared with clopidogrel, patients with asthma/COPD treated with ticagrelor may have an increased
risk of experiencing non-serious dyspnoea (3.29% ticagrelor versus 0.53% clopidogrel) and serious
dyspnoea (0.38% ticagrelor versus 0.00% clopidogrel). In absolute terms, this risk was higher than in
the overall PLATO population. Ticagrelor should be used with caution in patients with history of
asthma and/or COPD (see section 4.4).
About 30% of episodes resolved within 7 days. PLATO included patients with baseline congestive
heart failure, chronic obstructive pulmonary disease, or asthma; these patients, and the elderly, were
more likely to report dyspnoea.
For Possia, 0.9% of patients discontinued study drug because of
dyspnoea compared with 0.1% taking clopidogrel. The higher incidence of dyspnoea with Possia is not
associated with new or worsening heart or lung disease (see section 4.4). Possia does not affect tests of
pulmonary function.
Investigations
Creatinine elevations: In PLATO, serum creatinine concentration significantly increased by >30% in
25.5% of patients receiving ticagrelor compared to 21.3% of patients receiving clopidogrel and
by >50% in 8.3% of patients receiving ticagrelor compared to 6.7% of patients receiving clopidogrel.
Creatinine elevations by >50% were more pronounced in patients > 75 years (ticagrelor 13.6% versus
clopidogrel 8.8%), in patients with severe renal impairment at baseline (ticagrelor 17.8% versus
clopidogrel 12.5%) and in patients receiving concomitant treatment with ARBs (ticagrelor 11.2%
versus clopidogrel 7.1%). Within these subgroups renal-related serious adverse events and adverse
events leading to discontinuation of study drug were similar between treatment groups. The totality of
renal AEs reported were 4.9% for ticagrelor vs. 3.8% for clopidogrel, however a similar percent of
patients reported events considered by the investigators as causally related to treatment; 54 (0.6%) for
ticagrelor and 43 (0.5%) for clopidogrel.
Uric acid elevations: In PLATO, serum uric acid concentration increased to more than upper limit of
normal in 22% of patients receiving ticagrelor compared to 13% of patients receiving clopidogrel.
Mean serum uric acid concentration increased approximately 15% with ticagrelor compared to
approximately 7.5% with clopidogrel and after treatment was stopped, decreased to approximately
7% on ticagrelor but with no decrease observed for clopidogrel. The hyperuricaemia AEs reported
were 0.5% for ticagrelor vs. 0.2% for clopidogrel. Of these AEs 0.05% for ticagrelor vs. 0.02% for
clopidogrel were considered causally related by investigators. For gouty arthritis, the AEs reported
were 0.2% for ticagrelor vs 0.1% for clopidogrel; none of these adverse events were assessed as
causally related by investigators.
Ticagrelor is well tolerated in single doses up to 900 mg. Gastrointestinal toxicity was dose-limiting in
a single ascending dose study. Other clinically meaningful adverse reactions which may occur with
overdose include dyspnoea and ventricular pauses (see section 4.8).
In the event of overdose, observe for these potential adverse reactions and consider ECG monitoring
There is currently no known antidote to reverse the effects of Possia, and Possia is not expected to be
dialysable (see section 4.4). Treatment of overdose should follow local standard medical practice. The
expected effect of excessive Possia dosing is prolonged duration of bleeding risk associated with
platelet inhibition. If bleeding occurs appropriate supportive measures should be taken.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: Platelet aggregation inhibitors excluding heparin, ATC code: B01AC24
Mechanism of action
Possia contains ticagrelor a member of the chemical class cyclopentyltriazolopyrimidines (CPTP),
which is a selective adenosine diphosphate (ADP) receptor antagonist acting on the P2Y
12
ADP-receptor that can prevent ADP-mediated platelet activation and aggregation. Ticagrelor is orally
active, and reversibly interacts with the platelet P2Y
12
ADP-receptor. Ticagrelor does not interact with
the ADP binding site itself, but interacts with platelet P2Y
12
ADP-receptor to prevent signal
transduction.
Pharmacodynamic effects
Onset of Action
In patients with stable coronary artery disease on ASA, ticagrelor demonstrates a rapid onset of
pharmacological effect as demonstrated by a mean Inhibition of Platelet Aggregation (IPA) for
ticagrelor at 0.5 hours after 180 mg loading dose of about 41%, with the maximum IPA effect of
89% by 2-4 hours post dose, and maintained between 2-8 hours. 90% of patients had final extent IPA
>70% by 2 hours post dose.
Offset of Action
If a CABG procedure is planned, ticagrelor bleeding risk is increased compared to clopidogrel when
discontinued within less than 96 hours prior to procedure.
Switching data
Switching from clopidogrel to ticagrelor results in an absolute IPA increase of 26.4% and switching
from ticagrelor to clopidogrel results in an absolute IPA decrease of 24.5%. Patients can be switched
from clopidogrel to ticagrelor without any interruption of antiplatelet effect (see section 4.2).
Clinical efficacy and safety
The PLATO study included 18,624 patients who presented within 24 hours of onset of symptoms of
unstable angina (UA), non ST elevation myocardial infarction (NSTEMI) or ST elevation myocardial
infarction (STEMI), and were initially managed medically, or with percutaneous coronary intervention
(PCI), or with coronary artery bypass grafting (CABG) (see section 4.1).
On a background of daily ASA, ticagrelor 90 mg twice daily showed superiority to 75 mg daily
clopidogrel in preventing the composite endpoint of cardiovascular [CV] death, myocardial infarction
[MI], or stroke, with the difference driven by CV death and MI. Patients received a 300 mg loading
dose of clopidogrel (600 mg possible if having PCI) or 180 mg of ticagrelor.
The result appeared early (absolute risk reduction [ARR] 1.0% and Relative Risk Reduction [RRR] of
12% at 30 days), with a constant treatment effect over the entire 12 month period, yielding ARR
1.9% per year with RRR of 16%. This suggests it is appropriate to treat patients with ticagrelor for up
to 12 months (see section 4.2). Treating 54 ACS patients with ticagrelor instead of clopidogrel will
prevent 1 atherothrombotic event; treating 91 will prevent 1 CV death (see Figure 1 and Table 3).
The treatment effect of ticagrelor over clopidogrel appears consistent across many subgroups,
including weight; sex; medical history of diabetes mellitus, transient ischaemic attack or non-
haemorrhagic stroke, or revascularisation; concomitant therapies including heparins, GpIIb/IIIa
inhibitors and proton pump inhibitors (see section 4.5); final index event diagnosis (STEMI, NSTEMI,
or UA); and, treatment pathway intended at randomisation (invasive or medical).
A weakly significant treatment interaction was observed with region whereby the HR for the primary
endpoint favours ticagrelor in the rest of world but favours clopidogrel in North America, which
represented approximately 10% of the overall population studied (interaction p-value=0.045).
Exploratory analyses suggest a possible association with ASA dose such that reduced efficacy was
observed with ticagrelor with increasing ASA doses. Chronic daily ASA doses to accompany Possia
should be 75-150 mg (see section 4.2 and 4.4).
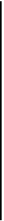
Figure 1 shows the estimate of the risk to the first occurrence of any event in the composite efficacy
endpoint.
Figure 1 – Time to first occurrence of CV death, MI and Stroke (PLATO)
Possia reduced the occurrence of the primary composite endpoint compared to clopidogrel in both the
UA/NSTEMI and STEMI population (Table 3).



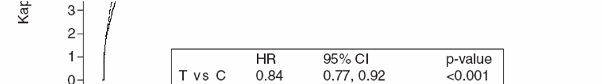

Table 3 -Outcome Events in PLATO
Possia
(% patients
with event)
N=9333
Clopidogrel
(% patients
with event)
N=9291
CV death, MI (excl.
silent MI) or stroke
All cause mortality,
MI (excl. silent MI),
or stroke
CV death, total MI,
stroke, SRI, RI, TIA,
or other ATE
c
0.0123
d
a
ARR = absolute risk reduction; RRR = relative risk reduction = (1-Hazard ratio) x 100%. A negative RRR indicates a
relative risk increase.
b
excluding silent myocardial infarction.
c
SRI = serious recurrent ischaemia; RI = recurrent ischaemia; TIA = transient ischaemic attack; ATE = arterial thrombotic
event. Total MI includes silent MI, with date of event set to date when discovered.
d
nominal significance value; all others are formally statistically significant by pre-defined hierarchical testing.
Holter Substudy
To study the occurrence of ventricular pauses and other arrhythmic episodes during PLATO,
investigators performed Holter monitoring in a subset of nearly 3000 patients, of whom
approximately 2000 had recordings both in the acute phase of their ACS and after one month. The
primary variable of interest was the occurrence of ventricular pauses ≥3 seconds. More patients had
ventricular pauses with ticagrelor (6.0%) than with clopidogrel (3.5%) in the acute phase; and
2.2% and 1.6% respectively after 1 month (see section 4.4). The increase in ventricular pauses in the
acute phase of ACS was more pronounced in ticagrelor patients with history of CHF (9.2% versus
5.4% in patients without CHF history; for clopidogrel patients, 4.0% in those with versus 3.6% in
those without CHF history) This imbalance did not occur at one month: 2.0% versus 2.1% for
ticagrelor patients with and without CHF history respectively; and 3.8% versus 1.4% with clopidogrel.
There were no adverse clinical consequences associated with this imbalance (including pacemaker
insertions) in this population of patients.
PLATO genetic substudy
CYP2C19 and ABCB1 genotyping of 10,285 patients in PLATO provided associations of genotype
groups with PLATO outcomes. The superiority of ticagrelor over clopidogrel in reducing major CV
events was not significantly affected by patient CYP2C19 or ABCB1 genotype. Similar to the overall
PLATO study, total PLATO Major bleeding did not differ between ticagrelor and clopidogrel,
regardless of CYP2C19 or ABCB1 genotype. Non-CABG PLATO Major bleeding was increased with
ticagrelor compared clopidogrel in patients with one or more CYP2C19 loss of function alleles, but
similar to clopidogrel in patients with no loss of function allele.
Combined efficacy and safety composite
A combined efficacy and safety composite (CV death, MI, stroke, or PLATO-defined ‘Total Major’
bleeding) indicates that the benefit in efficacy of Possia compared to clopidogrel is not offset by the
major bleeding events (ARR 1.4%, RRR 8%, HR 0.92; p=0.0257) over 12 months after ACS.
Definite stent
thrombosis
















Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with Possia
in all subsets of the paediatric population in the granted indication (see section 4.2 and 5.2).
5.2 Pharmacokinetic properties
Ticagrelor demonstrates linear pharmacokinetics and exposure to ticagrelor and the active metabolite
(AR-C124910XX) are approximately dose proportional up to 1260 mg.
Absorption
Absorption of ticagrelor is rapid with a median t
max
of approximately 1.5 hours. The formation of the
major circulating metabolite AR-C124910XX (also active) from ticagrelor is rapid with a median t
max
of approximately 2.5 hours. Following oral administration of ticagrelor 90 mg under fasted conditions,
C
max
is 529 ng/ml and AUC is 3451 ng*h/ml. The metabolite parent ratios are 0.28 for C
max
and 0.42
for AUC.
The mean absolute bioavailability of ticagrelor was estimated to be 36%. Ingestion of a high-fat meal
resulted in a 21% increase in ticagrelor AUC and 22% decrease in the active metabolite C
max
but had
no effect on ticagrelor C
max
or the AUC of the active metabolite. These small changes are considered
of minimal clinical significance; therefore, ticagrelor can be given with or without food. Ticagrelor as
well as the active metabolite are P-gp substrates.
Distribution
The steady state volume of distribution of ticagrelor is 87.5 l. Ticagrelor and the active metabolite is
extensively bound to human plasma protein (>99.7%).
Biotransformation
CYP3A4 is the major enzyme responsible for ticagrelor metabolism and the formation of the active
metabolite and their interactions with other CYP3A substrates ranges from activation through to
inhibition.
The major metabolite of ticagrelor is AR-C124910XX, which is also active as assessed by
in vitro
binding to the platelet P2Y
12
ADP-receptor. The systemic exposure to the active metabolite is
approximately 30-40% of that obtained for ticagrelor.
Elimination
The primary route of ticagrelor elimination is via hepatic metabolism. When radiolabeled ticagrelor is
administered, the mean recovery of radioactivity is approximately 84% (57.8% in faeces, 26.5% in
urine). Recoveries of ticagrelor and the active metabolite in urine were both less than 1% of the dose.
The primary route of elimination for the active metabolite is most likely via biliary secretion. The
mean t
1/2
was approximately 7 hours for ticagrelor and 8.5 hours for the active metabolite.
Elderly
Higher exposures to ticagrelor (approximately 25% for both C
max
and AUC) and the active metabolite
were observed in elderly (≥ 75years) ACS patients compared to younger patients by the population
pharmacokinetic analysis. These differences are not considered clinically significant (see section 4.2).
Paediatric
Ticagrelor has not been evaluated in a paediatric population (see section 4.2 and 5.1).
Gender
Higher exposures to ticagrelor and the active metabolite were observed in women compared to men.
These differences are not considered clinically significant.
Renal impairment
Exposure to ticagrelor and the active metabolite were approximately 20% lower in patients with severe
renal impairment (creatinine clearance <30 ml/min) compared to subjects with normal renal function
(see section 4.2).
Hepatic impairment
C
max
and AUC for ticagrelor were 12% and 23% higher in patients with mild hepatic impairment
compared to matched healthy subjects, respectively (see section 4.2). Ticagrelor has not been studied
in patients with moderate or severe hepatic impairment and its use in these patients is contraindicated
(see section 4.3 and 4.4).
Ethnicity
Patients of Asian descent have a 39% higher mean bioavailability compared to Caucasian patients.
Patients self-identified as Black had an 18% lower bioavailability of ticagrelor compared to Caucasian
patients. In clinical pharmacology studies, the exposure (C
max
and AUC) to ticagrelor in Japanese
subjects was approximately 40% (20% after adjusting for body weight) higher compared to that in
Caucasians.
5.3 Preclinical safety data
Preclinical data for ticagrelor and its major metabolite have not demonstrated unacceptable risk for
adverse effects for humans based on conventional studies of safety pharmacology, single and repeated
dose toxicity and genotoxic potential.
Gastrointestinal irritation was observed in several animal species at clinical relevant exposure levels
(see section 4.8).
In female rats, ticagrelor at high dose showed an increased incidence of uterine tumors
(adenocarcinomas) and an increased incidence of hepatic adenomas. The mechanism for uterine
tumors is likely hormonal imbalance which can lead to tumors in rats. The mechanism for the hepatic
adenomas is likely due to a rodent-specific enzyme induction in the liver. Thus, the carcinogenicity
findings are considered unlikely to be relevant for humans.
In rats minor developmental anomalies were seen at a maternal toxic dose (safety margin of 5.1). In
rabbits a slight delay in hepatic maturity and skeletal development was seen in foetuses from dams at
high dose without showing maternal toxicity (safety margin of 4.5).
Studies in rats and rabbits have shown reproductive toxicity, with slightly reduced maternal body
weight gain and reduced neonatal viability and birth weight, with delayed growth. Ticagrelor produced
irregular cycles (mostly extended cycles) in female rats, but did not affect overall fertility in male and
female rats. Pharmacokinetic studies performed with radio-labeled ticagrelor have shown that the
parent compound and its metabolites are excreted in the milk of rats (see section 4.6).
PHARMACEUTICAL PARTICULARS
Core
Mannitol (E421)
Dibasic calcium phosphate
Magnesium stearate (E470b)
Sodium starch glycolate
Hydroxypropyl-cellulose (E463)
Coating
Talc
Titanium dioxide (E171)
Ferric oxide yellow (E172)
Polyethylene-glycol 400
Hypromellose (E464)
6.4 Special precautions for storage
This medicinal product does not require any special storage conditions.
6.5 Nature and contents of container
• PVC-PVDC/Al transparent blister (with sun/moon symbols) of 10 tablets; cartons of 60 tablets
(6 blisters) and 180 tablets (18 blisters).
• PVC-PVDC/Al transparent calendar blister (with sun/moon symbols) of 14 tablets; cartons of
14 tablets (1 blister), 56 tablets (4 blisters), and 168 tablets (12 blisters).
• PVC-PVDC/Al perforated unit dose transparent blister of 10 tablets; cartons of 100x1 tablets
(10 blisters).
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
MARKETING AUTHORISATION HOLDER
AstraZeneca AB
S-151 85
Södertälje
Sweden
MARKETING AUTHORISATION NUMBER(S)
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency
http://www.ema.europa.eu
ANNEX II
A. MANUFACTURING AUTHORISATION HOLDER RESPONSIBLE
FOR BATCH RELEASE
B. CONDITIONS OF THE MARKETING AUTHORISATION
A. MANUFACTURING AUTHORISATION HOLDER RESPONSIBLE FOR BATCH
RELEASE
Name and address of the manufacturer responsible for batch release
AstraZeneca AB
Gärtunavägen
SE-151 85 Södertälje
Sweden
B. CONDITIONS OF THE MARKETING AUTHORISATION
Conditions or restrictions regarding supply and use imposed on the marketing
authorisation holder
Medicinal product subject to medical prescription.
Conditions or restrictions with regard to the safe and effective use of the medicinal
product
The MAH must ensure that the system of pharmacovigilance, as described in version 11 (21 June
2010) presented in Module 1.8.1. of the Marketing Authorisation Application, is in place and
functioning before and whilst the product is on the market.
The MAH commits to performing the studies and additional pharmacovigilance activities detailed in
the Pharmacovigilance Plan, as agreed in version 4 (21 September 2010) of the Risk Management Plan
(RMP) presented in Module 1.8.2. of the Marketing Authorisation Application and any subsequent
updates of the RMP agreed by the CHMP.
As per the CHMP Guideline on Risk Management Systems for medicinal products for human use, the
updated RMP should be submitted at the same time at the next Periodic Safety Update Report (PSUR).
In addition, an updated RMP should be submitted:
• When new information is received that may impact on the current Safety Specification,
Pharmacovigilance Plan or risk minimisation activities
• Within 60 days of an important (pharmacovigilance or risk minimisation) milestone being
reached
• At the request of the EMA.
ANNEX III
LABELLING AND PACKAGE LEAFLET
PARTICULARS TO APPEAR ON THE OUTER PACKAGING
CARTON OF 90 mg FILM-COATED TABLETS
NAME OF THE MEDICINAL PRODUCT
Possia 90 mg film-coated tablets
ticagrelor
STATEMENT OF ACTIVE SUBSTANCE(S)
Each film-coated tablet contains 90 mg ticagrelor
PHARMACEUTICAL FORM AND CONTENTS
14 film-coated tablets
56 film-coated tablets
60 film-coated tablets
100x1 film-coated tablets
168 film-coated tablets
180 film-coated tablets
METHOD AND ROUTE(S) OF ADMINISTRATION
Read the package leaflet before use.
Oral use
SPECIAL WARNING THAT THE MEDICINAL PRODUCT MUST BE STORED OUT
OF THE REACH AND SIGHT OF CHILDREN
Keep out of the reach and sight of children.
OTHER SPECIAL WARNING(S), IF NECESSARY
SPECIAL STORAGE CONDITIONS

























10. SPECIAL PRECAUTIONS FOR DISPOSAL OF UNUSED MEDICINAL PRODUCTS
OR WASTE MATERIALS DERIVED FROM SUCH MEDICINAL PRODUCTS, IF
APPROPRIATE
11. NAME AND ADDRESS OF THE MARKETING AUTHORISATION HOLDER
AstraZeneca AB
S-151 85
Södertälje
Sweden
12. MARKETING AUTHORISATION NUMBER(S)
14. GENERAL CLASSIFICATION FOR SUPPLY
Medicinal product subject to medical prescription.
16. INFORMATION IN BRAILLE
















MINIMUM PARTICULARS TO APPEAR ON BLISTERS OR STRIPS
CALENDAR BLISTER (14 TABLETS)
NAME OF THE MEDICINAL PRODUCT
Possia 90 mg tablets
ticagrelor
NAME OF THE MARKETING AUTHORISATION HOLDER
Mon Tue Wed Thu Fri Sat Sun
Sun/Moon symbol














PACKAGE LEAFLET: INFORMATION FOR THE USER
Possia 90 mg film-coated tablets
ticagrelor
Read all of this leaflet carefully before you start taking this medicine.
-
Keep this leaflet. You may need to read it again.
If you have any further questions, ask your doctor or pharmacist.
This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even
if their symptoms are the same as yours.
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet,
please tell your doctor or pharmacist.
What Possia is and what it is used for
WHAT POSSIA IS AND WHAT IT IS USED FOR
What Possia is
Possia contains the active substance called ticagrelor. This belongs to a group of medicines called
anti-platelet medicines.
How Possia works
Possia affects cells called ‘platelets’ (also called thrombocytes). These very small blood cells help stop
bleeding by clumping together to plug tiny holes in blood vessels that are cut or damaged.
However, platelets can also form clots inside diseased blood vessels in the heart and brain. This can be
very dangerous because:
• the clot can cut off the blood supply completely - this can cause a heart attack (myocardial
infarction) or stroke, or
• the clot can partly block the blood vessels to the heart - this reduces the blood flow to the heart
and can cause chest pain which comes and goes (called ‘unstable angina’).
Possia helps stop the clumping of platelets. This reduces the chance of a blood clot forming that can
reduce blood flow.
What Possia is used for
Possia is to be used in adults only. You have been given Possia because you have had:
• a heart attack, or
• unstable angina (angina or chest pain that is not well controlled).
Possia reduces the chances of you having another heart attack or a stroke or of dying from a disease
related to your heart or blood vessels.
Do not take Possia if:
• You are allergic (hypersensitive) to ticagrelor or any of the other ingredients of Possia (listed in
Section 6: Further information).
• You are bleeding now or have bled recently inside your body, such as bleeding in your stomach
or gut from an ulcer.
• You have moderate to severe liver disease
• You are taking any of the following medicines: ketoconazole (used to treat fungal infections),
clarithromycin (used to treat bacterial infections), nefazodone (an antidepressant), ritonavir and
atazanavir (used to treat HIV infection and AIDS).
• You have had a stroke caused by bleeding in the brain.
Do not take Possia if any of the above applies to you. If you are not sure, talk to your doctor or
pharmacist before taking Possia.
Take special care with Possia
Check with your doctor, pharmacist or dentist before taking Possia if:
• You have an increased risk of bleeding because of:
-
a recent serious injury
-
recent surgery (including dental work)
-
you have a condition that affects blood clotting
-
recent bleeding from your stomach or gut (such as a stomach ulcer or colon ‘polyps’)
• You are due to have surgery (including dental work) at any time while taking Possia. This is
because of the increased risk of bleeding. Your doctor may want you to stop taking Possia 7
days prior to surgery.
• Your heart rate is abnormally low (usually lower than 60 beats per minute) and you do not
already have in place a device that paces your heart (pacemaker).
• You have asthma or other lung problem or breathing difficulties.
• You have had a blood test that showed more than the usual amount of uric acid
If any of the above apply to you (or you are not sure), talk to your doctor, pharmacist or dentist before
taking Possia.
Children
Possia is not recommended for children and adolescents under 18 years.
Taking other medicines
Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines. This
includes medicines that you buy without a prescription, dietary supplements and herbal remedies. This
is because Possia can affect the way some medicines work and some medicines can have an effect on
Possia.
Tell your doctor or pharmacist if you are taking any of the following medicines:
• more than 40 mg daily of either simvastatin or lovastatin (medicines used to treat high
cholesterol)
• rifampicin (an antibiotic), phenytoin, carbamazepine and phenobarbital (used to control
seizures), dexamethasone (used to treat inflammatory and auto immune conditions), digoxin
(used to treat heart failure), cyclosporin (used to lessen your body’s defenses), quinidine and
diltiazem (used to treat abnormal heart rhythms), beta blockers and verapamil (used to treat high
blood pressure).
In particular, tell your doctor or pharmacist if you are taking any of the following medicines that
increase your risk of bleeding:
• ‘oral anticoagulants’ often referred to as ’blood thinners’ which include warfarin.
• non-steroidal anti-inflammatory drugs (abbreviated as NSAIDs) often taken as pain killers such
as ibuprofen and naproxen.
• selective serotonin reuptake inhibitors (abbreviated as SSRIs) taken as antidepressants such as
paroxetine, sertraline and citalopram
• other medicines such as ketoconazole (used to treat fungal infections), clarithromycin (used to
treat bacterial infections), nefazodone, (an antidepressant), ritonavir and atazanavir (used to treat
HIV infection and AIDS), cisapride (used to treat heartburn), ergot alkaloids (used to treat
migraines and headaches).
Also tell your doctor that because you are taking Possia, you may have an increased risk of bleeding if
your doctor gives you fibrinolytics, often called ‘clot dissolvers’, such as streptokinase or alteplase.
Taking Possia with food and drink
You can take Possia with or without food.
Pregnancy and breast-feeding
It is not recommended to use Possia if you are pregnant or may become pregnant. Women should use
appropriate contraceptive measures to avoid pregnancy while taking this medicine.
Talk to your doctor before taking Possia if you are breast-feeding. Your doctor will discuss with you
the benefits and risks of taking Possia during this time.
Ask your doctor or pharmacist for advice before taking any medicine, if you are pregnant or breast-
feeding.
Driving and using machines
Possia is not likely to affect your ability to drive or use machines.
Always take Possia exactly as your doctor has told you. You should talk with your doctor or
pharmacist if you are not sure.
How much to take
• The starting dose is two tablets at the same time (loading dose of 180 mg). This dose will
usually be given to you in the hospital.
• After this starting dose, the usual dose is one tablet of 90 mg twice a day for up to 12 months
unless your doctor tells you differently. Take Possia around the same time everyday (for
example, one tablet in the morning and one in the evening).
Your doctor will usually also tell you to take acetylsalicylic acid. This is a substance present in many
medicines used to prevent blood clotting. Your doctor will tell you how much to take (usually between
75-150 mg daily).
How to take Possia
• You can take the tablet with or without food.
• You can check when you last took a tablet of Possia by looking on the blister. There is a sun
(for the morning) and a moon (for the evening). This will tell you whether you have taken the
dose.
If you take more Possia than you should
If you take more Possia than you should, talk to a doctor or go to hospital straight away. Take the
medicine pack with you. You may be at increased risk of bleeding.
If you forget to take Possia
• If you forget to take a dose, just take your next dose as normal.
• Do not take a double dose (two doses at the same time) to make up for the forgotten dose.
If you stop taking Possia
Do not stop taking Possia without talking to your doctor. Take Possia on a regular basis and for as
long as your doctor keeps prescribing it. If you stop taking Possia, it may increase your chances of
having another heart attack or stroke or dying from a disease related to your heart or blood vessels.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Like all medicines, Possia can cause side effects, although not everybody gets them. The following
side effects may happen with this medicine:
The frequency of possible side effects listed below is defined using the following convention:
common (affects 1 to 10 users in 100); uncommon (affects 1 to 10 users in 1,000); rare (affects 1 to 10
users in 10,000)
See a doctor straight away if you notice any of the following – you may need urgent medical
treatment:
•
Signs of a stroke such as:
-
sudden numbness or weakness of your arm, leg or face, especially if only on one side of the
body
-
sudden confusion, difficulty speaking or understanding others
-
sudden difficulty in walking or loss of balance or co-ordination
-
suddenly feeling dizzy or sudden severe headache with no known cause
These are signs of a kind of stroke caused by bleeding into the brain. This is uncommon.
•
Bleeding
– some bleeding is common. However, severe bleeding is uncommon, but can be life
threatening. Bleeding of many different kinds can be increased, for example:
-
nosebleed (common)
-
blood in your urine (uncommon)
-
black stools or blood in your stools (common)
-
blood in your eye (uncommon)
-
coughing up or bringing up blood (uncommon)
-
vaginal bleeding that is heavier, or happens at different times, to your normal period
(menstrual) bleeding (uncommon)
-
bleeding after surgery or from cuts and wounds that is more than normal (common)
-
bleeding from your stomach lining (ulcer) (uncommon).
-
bleeding gums (uncommon)
-
blood in your ear (rare)
-
internal bleeding (rare)
-
bleeding into joints causing painful swelling (rare)
Discuss with your doctor if you notice any of the following:
•
Feeling short of breath
- this is common. It might be due to your heart disease or another
cause, or it might be a side effect of Possia. If your feeling of shortness of breath gets worse or
lasts a long time, tell your doctor. Your doctor will decide if it needs treatment or further
investigations.
Other possible side effects
Common (affects 1 to 10 users in 100)
• Bruising
Uncommon (affects 1 to 10 users in 1,000)
• Headache
• Feeling dizzy or like the room is spinning
• Abdominal pain
• Diarrhoea or indigestion
• Feeling or being sick
• Rash
• Itching
• Inflamed stomach (gastritis)
Rare (affects 1 to 10 users in 10,000)
• Constipation
• A tingling feeling
• Confusion
If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please
tell your doctor or pharmacist, but do not stop taking Possia until you have spoken to them.
Keep out of the reach and sight of children.
Do not use Possia after the expiry date, which is stated on the blister and carton after EXP. The expiry
date refers to the last day of that month.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to
dispose of medicines no longer required. These measures will help to protect the environment.
What Possia contains
• The active substance is ticagrelor. Each film-coated tablet contains 90 mg of ticagrelor.
• The other ingredients are:
Tablet core
: mannitol (E421), dibasic calcium phosphate, sodium starch glycolate,
hydroxypropyl-cellulose (E463), magnesium stearate (E470b)
Tablet film coating
: hypromellose (E464), titanium dioxide (E171), talc,
polyethylene--glycol 400, and ferric oxide yellow (E172).
What Possia looks like and contents of the pack
Film-coated tablet (tablet): The tablets are round, biconvex, yellow, film-coated marked with a “90”
above “T” on one side.
Possia is available in:
• standard blisters (with sun/moon symbols) in cartons of 60 and 180 tablets
• calendar blisters (with sun/moon symbols) in cartons of 14, 56 and 168 tablets
• perforated blisters in a carton of 100x1 tablets
Not all pack sizes may be marketed.
Marketing Authorisation Holder and Manufacturer
Marketing Authorisation Holder:
AstraZeneca AB
S-151 85
Södertälje
Sweden
Manufacturer:
AstraZeneca AB
Gärtunavägen
SE-151 85
Södertälje
Sweden
Manufacturer:
AstraZeneca UK Limited

Silk Road Business Park
Macclesfield, Cheshire, SK10 2NA
United Kingdom
For any information about this medicine, please contact the local representative of the Marketing
Authorisation Holder:
België/Belgique/Belgien
NV AstraZeneca SA
Luxembourg/Luxemburg
NV AstraZeneca SA
Tél/Tel: + 32 2 370 48 11
България
T
П
AstraZeneca UK Limited
Te
л
.: +359 2 971 25 33
Magyarország
AstraZeneca kft
Tel.: + 36 1 883 6500
Česká republika
AstraZeneca Czech Republic s.r.o
Tel: +420 222 807 111
Malta
Associated Drug Co. Ltd
Tel: + 356 2277 8000
Danmark
AstraZeneca A/S
Tlf: +45 43 66 64 62
Nederland
AstraZeneca BV
Tel: +31 79 363 2222
Deutschland
AstraZeneca GmbH
Tel: + 49 41 03 7080
Norge
AstraZeneca AS
Tlf: + 47 21 00 64 00
Eesti
AstraZeneca
Tel: +372 654 96 00
Österreich
AstraZeneca Österreich GmbH
Tel: +43 1 711 31 0
Ελλάδα
AstraZeneca A.E.
Τηλ: + 30 2 10 68 71 500
Polska
AstraZeneca Pharma Poland Sp. z o.o.
Tel.: + 48 22 874 35 00
España
Laboratorios Almirall, S.A.
Tel: + 34 93 31 28 748
Portugal
Medinfar Produtos Farmacêuticos, S.A.
Tel: + 351 21 499 74 00
France
AstraZeneca
Tél: + 33 1 41 29 40 00
România
AstraZeneca Pharma SRL
Tel: + 40 21 317 60 41
Ireland
AstraZeneca Pharmaceuticals (Ireland) Ltd
Tel: + 353 1 609 7100
Slovenija
AstraZeneca UK Limited
Tel: + 386 1 51 35 600
Ísland
Vistor hf
Sími: + 354 535 7000
Slovenská republika
AstraZeneca AB o.z.
Tel: + 421 2 5737 7777
Italia
AstraZeneca S.p.A.
Tel: + 39 02 980111
Suomi/Finland
AstraZeneca Oy
Puh/Tel: + 358 10 23 010
Κύπρος
Αλέκτωρ Φαρµακευτική Λτδ

Latvija
AstraZeneca AB pārstāvniecība Latvijā
Tel: + 371 67377 100
United Kingdom
AstraZeneca UK Ltd
Tel: + 44 1582 836 836
Lietuva
UAB AstraZeneca
Tel: +370 5 2660550
This leaflet was last approved in
Detailed information on this medicine is available on the European Medicines Agency web site:
http://www.ema.europa.eu
.
Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/possia.html
Copyright © 1995-2021 ITA all rights reserved.
|








































































































































 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































