Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
REYATAZ 100 mg hard capsules
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each capsule contains 100 mg of atazanavir (as sulphate)
Excipient: 54.79 mg of lactose per capsule.
For a full list of excipients, see section 6.1.
Hard capsule
Opaque blue and white capsule printed with white and blue inks, with "BMS 100 mg" on one half and
with "3623" on the other half.
4.1 Therapeutic indications
REYATAZ capsules, co-administered with low dose ritonavir, are indicated for the treatment of
HIV-1 infected adults and paediatric patients 6 years of age and older in combination with other
antiretroviral medicinal products.
Based on available virological and clinical data from adult patients, no benefit is expected in patients
with strains resistant to multiple protease inhibitors (
The choice of REYATAZ in treatment experienced adult and paediatric patients should be based on
individual viral resistance testing and the patient’s treatment history (see sections 4.4 and 5.1).
4.2 Posology and method of administration
Therapy should be initiated by a physician experienced in the management of HIV infection.
Adults:
the recommended dose of REYATAZ capsules is 300 mg once daily taken with ritonavir
100 mg once daily and with food. Ritonavir is used as a booster of atazanavir pharmacokinetics
(see sections 4.5 and 5.1).
Paediatric patients (6 years to less than 18 years of age):
The dose of REYATAZ capsules for
paediatric patients is based on body weight as shown in Table 1 and should not exceed the
recommended adult dose. REYATAZ capsules must be taken with ritonavir and have to be taken with
food.
4 PI mutations). There are very limited data
available from children aged 6 to less than 18 years (see sections 4.4 and 5.1).
Table 1: Dose for Paediatric Patients (6 years to less than 18 years of age) for REYATAZ
capsules with ritonavir
Body Weight (kg)
a
Ritonavir capsules, tablets or oral solution.
b
Ritonavir oral solution no lower than 80 mg and not more than 100 mg may be used for paediatric
patients from 15 kg to less than 20 kg who cannot swallow ritonavir capsules/tablets.
The available data do not support the use of REYATAZ in combination with low dose ritonavir in
paediatric patients weighing less than 15 kg.
Paediatric patients (less than 6 years of age):
REYAYAZ is not recommended in paediatric patients
less than 6 years of age due to insufficient data on pharmacokinetics, safety, and efficacy. REYATAZ
has not been studied in children less than 3 months of age and is not recommended especially taking
into account the potential risk of kernicterus.
Patients with renal impairment:
no dosage adjustment is needed. REYATAZ with ritonavir is not
recommended in patients undergoing haemodialysis (see sections 4.4 and 5.2).
Patients with hepatic impairment:
REYATAZ with ritonavir has not been studied in patients with
hepatic impairment. REYATAZ with ritonavir should be used with caution in patients with mild
hepatic impairment. REYATAZ must not be used in patients with moderate to severe hepatic
impairment (see sections 4.3, 4.4, and 5.2).
Method of administration
: for oral administration. The capsules should be swallowed whole.
REYATAZ oral powder is available for adult patients who are unable to swallow capsules
(see Summary of Product Characteristics for REYATAZ oral powder). REYATAZ oral powder must
not be used in paediatric patients unable to swallow capsules due to insufficient data on
pharmacokinetics, safety, and efficacy.
Hypersensitivity to the active substance or to any of the excipients (see section 6.1).
Patients with moderate to severe hepatic insufficiency (see sections 4.2 and 4.4).
Combination of rifampicin and REYATAZ with concomitant low-dose ritonavir is contraindicated
(see section 4.5).
The PDE5 inhibitor sildenafil is contraindicated when used for the treatment of pulmonary arterial
hypertension (PAH) only (see section 4.5). For co-administration of sildenafil for the treatment of
erectile dysfunction see section 4.4 and section 4.5.
REYATAZ with ritonavir must not be used in combination with medicinal products that are substrates
of the CYP3A4 isoform of cytochrome P450 and have narrow therapeutic windows (e.g., alfuzosin,
astemizole, terfenadine, cisapride, pimozide, quinidine, bepridil, triazolam, midazolam administered
orally (for caution on parenterally administered midazolam, see section 4.5),
and ergot alkaloids,
particularly, ergotamine, dihydroergotamine, ergonovine, methylergonovine) (see section 4.5).
REYATAZ must not be used in combination with products containing St. John’s wort (
Hypericum
perforatum
) (see section 4.5).

4.4 Special warnings and precautions for use
Patients should be advised that current antiretroviral therapy has not been proven to prevent the risk of
transmission of HIV to others through blood or sexual contact. Appropriate precautions should
continue to be employed.
Co-administration of REYATAZ with ritonavir at doses greater than 100 mg once daily has not been
clinically evaluated. The use of higher ritonavir doses may alter the safety profile of atazanavir
(cardiac effects, hyperbilirubinaemia) and therefore is not recommended. Only when atazanavir with
ritonavir is co-administered with efavirenz, a dose increase of ritonavir to 200 mg once daily could be
considered. In this instance, close clinical monitoring is warranted (see Interaction with other
Medicinal Products below).
Patients with coexisting conditions
Atazanavir is primarily hepatically metabolised and increased plasma concentrations were observed in
patients with hepatic impairment
(see sections 4.2 and 4.3). The safety and efficacy of REYATAZ has
not been established in patients with significant underlying liver disorders. Patients with chronic
hepatitis B or C and treated with combination antiretroviral therapy are at an increased risk for severe
and potentially fatal hepatic adverse reactions. In case of concomitant antiviral therapy for hepatitis B
or C, please refer also to the relevant Summary of Product Characteristics for these medicinal products
(see section 4.8).
Patients with pre-existing liver dysfunction, including chronic active hepatitis, have an increased
frequency of liver function abnormalities during combination antiretroviral therapy and should be
monitored according to standard practice. If there is evidence of worsening liver disease in such
patients, interruption or discontinuation of treatment must be considered.
No dosage adjustment is needed in patients with renal impairment. However, REYATAZ with
ritonavir is not recommended in patients undergoing haemodialysis (see sections 4.2 and 5.2).
Dose related asymptomatic prolongations in PR interval with REYATAZ have been observed in
clinical studies. Caution should be used with medicinal products known to induce PR prolongations. In
patients with pre-existing conduction problems (second degree or higher atrioventricular or complex
bundle-branch block), REYATAZ should be used with caution and only if the benefits exceed the risk
(see section 5.1). Particular caution should be used when prescribing REYATAZ in association with
medicinal products which have the potential to increase the QT interval and/or in patients with
pre-existing risk factors (bradycardia, long congenital QT, electrolyte imbalances (see sections 4.8 and
5.3).
There have been reports of increased bleeding, including spontaneous skin haematomas and
haemarthroses, in type A and B haemophiliac patients treated with protease inhibitors. In some
patients additional factor VIII was given. In more than half of the reported cases, treatment with
protease inhibitors was continued or reintroduced if treatment had been discontinued. A causal
relationship has been suggested, although the mechanism of action has not been elucidated.
Haemophiliac patients should therefore be made aware of the possibility of increased bleeding.
Fat redistribution and metabolic disorders
Combination antiretroviral therapy has been associated with the redistribution of body fat
(lipodystrophy) in HIV patients. The long-term consequences of these events are currently unknown.
Knowledge about the mechanism is incomplete. A connection between visceral lipomatosis and
protease inhibitors and lipoatrophy and nucleoside reverse transcriptase inhibitors has been
hypothesised. A higher risk of lipodystrophy has been associated with individual factors such as older
age, and with drug related factors such as longer duration of antiretroviral treatment and associated
metabolic disturbances. Clinical examination should include evaluation for physical signs of fat
redistribution.
Combination antiretroviral therapy (CART), including REYATAZ (with or without ritonavir)-based
CART, is associated with dyslipidaemia. Consideration should be given to the measurement of fasting
serum lipids and blood glucose. Lipid disorders should be managed as clinically appropriate
(see section 4.8).
In clinical studies, REYATAZ (with or without ritonavir) has been shown to induce dyslipidaemia to a
lesser extent than comparators. The clinical impact of such findings has not been demonstrated in the
absence of specific studies on cardiovascular risk. The selection of antiretroviral therapy must be
guided principally by antiviral efficacy. Consultation with standard guidelines for management of
dyslipidaemia is recommended.
Hyperglycaemia
New onset diabetes mellitus, hyperglycaemia, and exacerbation of existing diabetes mellitus have been
reported in patients receiving protease inhibitors. In some of these, the hyperglycaemia was severe and
in some cases also associated with ketoacidosis. Many patients had confounding medical conditions,
some of which required therapy with medicinal products that have been associated with development
of diabetes or hyperglycaemia.
Hyperbilirubinaemia
Reversible elevations in indirect (unconjugated) bilirubin related to inhibition of UDP-glucuronosyl
transferase (UGT) have occurred in patients receiving REYATAZ (see section 4.8). Hepatic
transaminase elevations that occur with elevated bilirubin in patients receiving REYATAZ should be
evaluated for alternative etiologies. Alternative antiretroviral therapy to REYATAZ may be
considered if jaundice or scleral icterus is unacceptable to a patient. Dose reduction of atazanavir is not
recommended because it may result in a loss of therapeutic effect and development of resistance.
Indinavir is also associated with indirect (unconjugated) hyperbilirubinaemia due to inhibition of
UGT. Combinations of REYATAZ and indinavir have not been studied and co-administration of these
medicinal products is not recommended (see section 4.5).
Nephrolithiasis
Nephrolithiasis has been reported in patients receiving REYATAZ (see section 4.8). If signs or
symptoms of nephrolithiasis occur, temporary interruption or discontinuation of treatment may be
considered.
Immune reactivation syndrome
In HIV-infected patients with severe immune deficiency at the time of institution of combination
antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic
pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically,
such reactions have been observed within the first few weeks or months of initiation of CART.
Relevant examples are cytomegalovirus retinitis, generalised and/or focal mycobacterial infections,
and
Pneumocystis carinii
pneumonia. Any inflammatory symptoms should be evaluated and treatment
instituted when necessary.
Osteonecrosis
Although the etiology is considered to be multifactorial (including corticosteroid use, alcohol
consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been
reported particularly in patients with advanced HIV-disease and/or long-term exposure to combination
antiretroviral therapy (CART). Patients should be advised to seek medical advice if they experience
joint aches and pain, joint stiffness or difficulty in movement.
Interactions with other medicinal products
Co-administration of REYATAZ with simvastatin or lovastatin is not recommended (see section 4.5).
Co-administration of REYATAZ with nevirapine or efavirenz is not recommended (see section 4.5).
If the co-administration of REYATAZ with an NNRTI is required, an increase in the dose of both
REYATAZ and ritonavir to 400 mg and 200 mg, respectively, in combination with efavirenz could be
considered with close clinical monitoring.
Atazanavir is metabolised principally by CYP3A4. Co-administration of REYATAZ with ritonavir
and medicinal products that induce CYP3A4 is not recommended (see sections 4.3 and 4.5).
PDE5 inhibitors used for the treatment of erectile dysfunction: particular caution should be used when
prescribing PDE5-inhibitors (sildenafil, tadalafil, or vardenafil) for the treatment of erectile
dysfunction in patients receiving REYATAZ with concomitant low-dose ritonavir. Co-administration
of REYATAZ with these medicinal products is expected to substantially increase their concentrations
and may result in PDE5-associated adverse events such as hypotension, visual changes and priapism
(see section 4.5).
Co-administration of voriconazole and REYATAZ with ritonavir is not recommended unless an
assessment of the benefit/risk justifies the use of voriconazole (see section 4.5).
Concomitant use of REYATAZ/ritonavir and fluticasone or other glucocorticoids that are metabolized
by CYP3A4 is not recommended unless the potential benefit of treatment outweighs the risk of
systemic corticosteroid effects, including Cushing's syndrome and adrenal suppression
(see section 4.5).
Concomitant use of salmeterol and REYATAZ/ritonavir may result in increased cardiovascular
adverse events associated with salmeterol. Co-administration of salmeterol and REYATAZ is not
recommended (see section 4.5).
The absorption of atazanavir may be reduced in situations where gastric pH is increased irrespective of
cause.
Co-administration of REYATAZ with proton pump inhibitors is not recommended (see section 4.5). If
the combination of REYATAZ with a proton pump inhibitor is judged unavoidable, close clinical
monitoring is recommended in combination with an increase in the dose of REYATAZ to 400 mg with
100 mg of ritonavir; doses of proton pump inhibitors comparable to omeprazole 20 mg should not be
exceeded.
Co-administration of REYATAZ/ritonavir in combination with tenofovir and an H
2
-receptor
antagonist should be avoided (see section 4.5).
Lactose
Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or
glucose-galactose malabsorption should not take this medicinal product.
Paediatric population
Safety:
Asymptomatic PR interval prolongation was more frequent in paediatric patients than adults.
Asymptomatic first- and second-degree AV block was reported in paediatric patients (see section 4.8).
Caution should be used with medicinal products known to induce PR prolongations. In paediatric
patients with pre-existing conduction problems (second degree or higher atrioventricular or complex
bundle-branch block), REYATAZ should be used with caution and only if the benefits exceed the risk.
Cardiac monitoring is recommended based on the presence of clinical findings (e.g., bradycardia).
Efficacy
Atazanavir/ritonavir is not effective in viral strains harbouring multiple mutations of resistance. While
in adults no benefit can be expected in patients with
4 PI mutations, in treatment experienced
children even lower numbers of PI mutations may be predictive of a lack of benefit (see section 5.1).
4.5 Interaction with other medicinal products and other forms of interaction
When REYATAZ and ritonavir are co-administered, the metabolic drug interaction profile for
ritonavir may predominate because ritonavir is a more potent CYP3A4 inhibitor than atazanavir. The
Summary of Product Characteristics for ritonavir must be consulted before initiation of therapy with
REYATAZ and ritonavir.
Atazanavir is metabolised in the liver through CYP3A4. It inhibits CYP3A4. Therefore, REYATAZ
with ritonavir is contraindicated with medicinal products that are substrates of CYP3A4 and have a
narrow therapeutic index: astemizole, terfenadine, cisapride, pimozide, quinidine, bepridil, triazolam,
orally administered midazolam, and ergot alkaloids, particularly ergotamine and dihydroergotamine
(see section 4.3).
Other interactions
Interactions between atazanavir/ritonavir and protease inhibitors, antiretroviral agents other than
protease inhibitors, and other non-antiretroviral medicinal products are listed in the tables below
(increase is indicated as “↑”, decrease as “↓”, no change as “↔”, twice daily as “BID” and once daily
as “QD”). If available, 90% confidence intervals (CI) are shown in parentheses. The studies presented
in Table 2 were conducted in healthy subjects unless otherwise noted. Of importance, many studies
were conducted with unboosted atazanavir, which is not the approved regimen of atazanavir.
Table 2: Interactions between REYATAZ and other medicinal products
Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
ANTI-INFECTIVES
Antiretrovirals
Protease inhibitors:
The co-administration of REYATAZ/ritonavir and other protease inhibitors has not been studied but would be
expected to increase exposure to other protease inhibitors. Therefore, such co-administration is not recommended.
Ritonavir 100 mg QD
(atazanavir 300 mg QD)
studies conducted in HIV-
infected patients
Ritonavir 100 mg once
daily is used as a
booster of atazanavir
pharmacokinetics.
* In a combined analysis, atazanavir 300 mg and ritonavir 100 mg
(n=33) was compared to atazanavir 400 mg without ritonavir (n=28).
The mechanism of interaction between atazanavir and ritonavir is
CYP3A4 inhibition.
Indinavir is associated with indirect unconjugated hyperbilirubinaemia
due to inhibition of UGT.
Co-administration of
REYATAZ/ritonavir
and indinavir is not
recommended (see
section 4.4).
Nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs)
Lamivudine 150 mg BID +
zidovudine 300 mg BID
(atazanavir 400 mg QD)
No significant effect on lamivudine and zidovudine concentrations was
observed.
Based on these data
and because ritonavir
is not expected to have
a significant impact on
the pharmacokinetics
of NRTIs, the
co-administration of
REYATAZ/ritonavir
with these medicinal
products is not
expected to
significantly alter the
exposure of the co-
administered drugs.
The co-administration of REYATAZ/ ritonavir with abacavir is not
expected to significantly alter the exposure of abacavir.
Didanosine (buffered tablets)
200 mg/stavudine 40 mg, both
single dose (atazanavir 400 mg
Didanosine should be
taken at the fasted state
2 hours after











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
atazanavir,
simultaneous
administration
with ddI+d4T
(fasted)
REYATAZ/ritonavir
taken with food. The
co-administration of
REYATAZ/ritonavir
with stavudine is not
expected to
significantly alter the
exposure of stavudine.
atazanavir, dosed 1
hr after ddI+d4T
(fasted)
Atazanavir concentrations were greatly decreased when co-administered
with didanosine (buffered tablets) and stavudine. The mechanism of
interaction is a reduced solubility of atazanavir with increasing pH related
to the presence of anti-acid agent in didanosine buffered tablets.
No significant effect on didanosine and stavudine concentrations was
observed.
Didanosine (enteric coated
capsules) 400 mg single dose
(atazanavir 300 mg QD with
ritonavir 100 mg QD)
↑1.25
(0.92, 1.69)
No significant effect on atazanavir concentrations was observed when
administered with enteric-coated didanosine, but administration with food
decreased didanosine concentrations.
Tenofovir disoproxil fumarate
300 mg QD (atazanavir 300
mg QD with ritonavir 100 mg
QD) studies conducted in HIV-
infected patients
* In a combined analysis from several clinical studies,
atazanavir/ritonavir 300/100 mg co-administered with tenofovir
disoproxil fumarate 300 mg (n=39) was compared to
atazanavir/ritonavir 300/100 mg (n=33).
The efficacy of REYATAZ/ritonavir in combination with tenofovir in
treatment-experienced patients has been demonstrated in clinical study
045 and in treatment naive patients in clinical study 138 (see sections
4.8 and 5.1). The mechanism of interaction between atazanavir and
tenofovir is unknown.
Tenofovir disoproxil fumarate
300 mg QD (atazanavir 300
mg QD with ritonavir 100 mg
QD)
tenofovir
disoproxil
fumarate
Patients should be
closely monitored for
tenofovir-associated
adverse events,
including renal
disorders.
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Efavirenz 600 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (pm):
all administered
with food
Co-administration of
efavirenz with
REYATAZ/ritonavir is
not recommended (see
section 4.4)
Efavirenz 600 mg QD
(atazanavir 400 mg QD with
ritonavir 200 mg QD)
↔1.12*/**
(0.84, 1.49)
* When compared to REYATAZ 300 mg/ritonavir 100 mg once daily in
the evening without efavirenz. This decrease in atazanavir C
min
, might
negatively impact the efficacy of atazanavir. The mechanism of
efavirenz/atazanavir interaction is CYP3A4 induction.
** based on historical comparison.
Nevirapine 200 mg BID
(atazanavir 400 mg QD with
ritonavir 100 mg QD) study
conducted in HIV infected
patients
Co-administration of
nevirapine with
REYATAZ/ritonavir is
not recommended (see
section 4.4)
↓0.41*
(0.27, 0.60)
* When compared to REYATAZ 300 mg and ritonavir 100 mg without
nevirapine. This decrease in atazanavir C
min
, might negatively impact
the efficacy of atazanavir. The mechanism of nevirapine/atazanavir
interaction is CYP3A4 induction.
Integrase Inhibitors
Raltegravir 400 mg BID
(atazanavir/ritonavir)
No dose adjustment
required for Isentress.
The mechanism is UGT1A1 inhibition.
atazanavir (pm):
all administered
with food











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
Antibiotics
Clarithromycin 500 mg BID
(atazanavir 400 mg QD)
No recommendation
regarding dose
reduction can be made;
therefore, caution
should be exercised if
REYATAZ/ritonavir is
co-administered with
clarithromycin.
A dose reduction of clarithromycin may result in subtherapeutic
concentrations of 14-OH clarithromycin. The mechanism of the
clarithromycin/atazanavir interaction is CYP3A4 inhibition.
Antifungals
Ketoconazole 200 mg QD
(atazanavir 400 mg QD)
No significant effect on atazanavir concentrations was observed.
Ketoconazole and
itraconazole should be
used cautiously with
REYATAZ/ritonavir.
High doses of
ketoconazole and
itraconazole (>200
mg/day) are not
recommended.
Itraconazole, like ketoconazole, is a potent inhibitor as well as a
substrate of CYP3A4.
Based on data obtained with other boosted PIs and ketoconazole, where
ketoconazole AUC showed a 3-fold increase, REYATAZ/ritonavir is
expected to increase ketoconazole or itraconazole concentrations.
Co-administration of REYATAZ/ritonavir and voriconazole has not
been studied.
Co-administration of
voriconazole and
REYATAZ/ritonavir is
not recommended
unless an assessment
of the benefit/risk to
the patient justifies the
use of voriconazole
(see section 4.4).
Patients should be
carefully monitored for
adverse events and/or
loss of efficacy during
the co-administration
of voriconazole and
REYATAZ/ritonavir.
The effect of co-administration of oral voriconazole and low dose (100
mg) oral ritonavir was investigated in healthy volunteers. Low doses of
ritonavir (100 mg BID) decreased the C
max
and AUC of voriconazole
(90% CI) by an average of 24% (↓9% to ↓36%) and 39% (↓22% to
↓52%), respectively. Administration of voriconazole resulted in a minor
decrease in steady state C
max
and AUC of ritonavir (90% CI) with an
average of 24% (↓6% to ↓39%) and 14% (↓26% to ↑1%), respectively.
Fluconazole 200 mg QD
(atazanavir 300 mg and
ritonavir 100 mg QD)
Atazanavir and fluconazole concentrations were not significantly
modified when REYATAZ/ritonavir was co-administered with
fluconazole.
No dosage adjustments
are needed for
REYATAZ/ritonavir
and fluconazole.
Antimycobacterial
Rifabutin 150 mg twice weekly
(atazanavir 300 mg and
ritonavir 100 mg QD)
When given with
REYATAZ/ritonavir,
the recommended dose
of rifabutin is 150 mg
3 times per week on set
days (for example
Monday-Wednesday-
Friday). Increased
monitoring for
rifabutin-associated
adverse reactions
including neutropenia
and uveitis is
warranted due to an
expected increase in
exposure to rifabutin.
Further dosage
reduction of rifabutin
to 150 mg twice
weekly on set days is
recommended for
25-O-desacetyl-
rifabutin
** When compared to rifabutin 150 mg QD alone. Total rifabutin and
25-O-desacetyl-rifabutin AUC: ↑2.19 (1.78, 2.69).
In previous studies, the pharmacokinetics of atazanavir was not altered
by rifabutin.











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
patients in whom the
150 mg dose 3 times
per week is not
tolerated. It should be
kept in mind that the
twice weekly dosage of
150 mg may not
provide an optimal
exposure to rifabutin
thus leading to a risk of
rifamycin resistance
and a treatment failure.
No dose adjustment is
needed for
REYATAZ/ritonavir.
Rifampicin is a strong CYP3A4 inducer and has been shown to cause a 72%
decrease in atazanavir AUC which can result in virological failure and
resistance development. During attempts to overcome the decreased exposure
by increasing the dose of REYATAZ or other protease inhibitors with
ritonavir, a high frequency of liver reactions was seen.
The combination of
rifampicin and
REYATAZ with
concomitant low-dose
ritonavir is
contraindicated
(see section 4.3).
ACID REDUCING AGENTS
H
2
-Receptor antagonists
For patients not
taking tenofovir,
if
REYATAZ 300
mg/ritonavir 100 mg
and H
2
-receptor
antagonists are
co-administered, a
dose equivalent to
famotidine 20 mg BID
should not be
exceeded. If a higher
dose of an H
2
-receptor
antagonist is required
(eg, famotidine 40 mg
BID or equivalent) an
increase of the
REYATAZ/ritonavir
dose from 300/100 mg
to 400/100 mg can be
considered.
In HIV-infected patients with atazanavir/ritonavir at
the recommended dose 300/100 mg QD
In Healthy volunteers with atazanavir/ritonavir at an
increased dose of 400/100 mg QD
atazanavir ↔1.03
(0.86, 1.22)
In HIV-infected patients with atazanavir/ritonavir at
the recommended dose of 300/100 mg QD
For patients who are
taking tenofovir,
Co-administration of
REYATAZ/ritonavir in
combination with
tenofovir and an
H
2
-receptor antagonist
should be avoided
(see section 4.4). If the
combination of
REYATAZ/ritonavir
with both tenofovir and
an H
2
-receptor
antagonist is judged
unavoidable, close
clinical monitoring is
recommended. A dose
increase of REYATAZ
to 400 mg with 100 mg
of ritonavir may be
atazanavir ↓0.79*
(0.66, 0.96)
atazanavir ↓0.76*
(0.64, 0.89)
* When compared to atazanavir 300 mg QD with ritonavir 100 mg QD
and tenofovir disoproxil fumarate 300 mg all as a single dose with food.
When compared to atazanavir 300 mg with ritonavir 100 mg
without
tenofovir
, atazanavir concentrations are expected to be additionally
decreased by about 20%.
The mechanism of interaction is decreased solubility of atazanavir as
intra-gastric pH increases with H
2
blockers.















Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
considered but is still
under evaluation.
Omeprazole 40 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (am): 2
hr after
omeprazole
Co-administration of
REYATAZ/ritonavir
with proton pump
inhibitors is not
recommended. If the
combination of
REYATAZ/ritonavir
with a proton pump
inhibitor is judged
unavoidable, close
clinical monitoring is
recommended in
combination with an
increase in the dose of
REYATAZ to 400 mg
with 100 mg of
ritonavir; doses of
proton pump inhibitors
comparable to
omeprazole 20 mg
should not be exceeded
(see section 4.4).
Omeprazole 20 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (am): 1
hr after
omeprazole
* When compared to atazanavir 300 mg QD with ritonavir 100 mg QD
The decrease in AUC, C
max
, and C
min
was not mitigated when an
increased dose of REYATAZ/ritonavir (400/100 mg once daily) was
temporally separated from omeprazole by 12 hours. Although not
studied, similar results are expected with other proton pump inhibitors.
This decrease in atazanavir exposure might negatively impact the
efficacy of atazanavir. The mechanism of interaction is decreased
solubility of atazanavir as intra-gastric pH increases with proton pump
inhibitors.
Antacids and medicinal
products containing buffers
Reduced plasma concentrations of atazanavir may be the consequence of
increased gastric pH if antacids, including buffered medicinal products,
are administered with REYATAZ/ritonavir.
REYATAZ/ritonavir
should be administered
2 hours before or 1
hour after antacids or
buffered medicinal
products.
ALPHA 1-ADRENORECEPTOR ANTAGONIST
Alfuzosin
Potential for increased alfuzosin concentrations which can result in
hypotension. The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Co-administration of
REYATAZ/ritonavir
with alfuzosin is
contraindicated (see
section 4.3)
Co-administration with REYATAZ/ritonavir has the potential to
produce a decrease or, less often, an increase in INR (International
Normalised Ratio).
It is recommended that
the INR be monitored
carefully during
treatment with
REYATAZ/ritonavir,
especially when
commencing therapy.
ANTINEOPLASTICS AND IMMUNOSUPRESSANTS
Atazanavir inhibits UGT and may interfere with the metabolism of
irinotecan, resulting in increased irinotecan toxicities.
If REYATAZ/ritonavir
is co-administered with
irinotecan, patients
should be closely
monitored for adverse
events related to
irinotecan.
Cyclosporin
Tacrolimus
Sirolimus
Concentrations of these immunosuppressants may be increased when
co-administered with REYATAZ/ritonavir due to CYP3A4 inhibition.
More frequent
therapeutic
concentration
monitoring of these
medicinal products is
recommended until
plasma levels have
been stabilised.














Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
Amiodarone,
Systemic lidocaine,
Quinidine
Concentrations of these antiarrhythmics may be increased when
co-administered with REYATAZ/ritonavir. The mechanism of
amiodarone or systemic lidocaine/atazanavir interaction is CYP3A
inhibition. Quinidine has a narrow therapeutic window and is
contraindicated due to potential inhibition of CYP3A by
REYATAZ/ritonavir.
Caution is warranted
and therapeutic
concentration
monitoring is
recommended when
available. The
concomitant use of
quinidine is
contraindicated
(see section 4.3).
REYATAZ/ritonavir should not be used in combination with medicinal
products that are substrates of CYP3A4 and have a narrow therapeutic
index.
Co-administration with
bepridil is
contraindicated (see
section 4.3)
Diltiazem 180 mg QD
(atazanavir 400 mg QD)
An initial dose
reduction of diltiazem
by 50% is
recommended, with
subsequent titration as
needed and ECG
monitoring.
No significant effect on atazanavir concentrations was observed. There
was an increase in the maximum PR interval compared to atazanavir
alone. Co-administration of diltiazem and REYATAZ/ritonavir has not
been studied. The mechanism of diltiazem/atazanavir interaction is
CYP3A4 inhibition.
Serum concentrations of verapamil may be increased by
REYATAZ/ritonavir due to CYP3A4 inhibition.
Caution should be
exercised when
verapamil is
co-administered with
REYATAZ/ritonavir.
Fluticasone propionate
intranasal 50 µg 4 times daily
for 7 days (ritonavir 100 mg
capsules BID)
The fluticasone propionate plasma levels increased significantly,
whereas the intrinsic cortisol levels decreased by approximately 86%
(90% confidence interval 82-89%) Greater effects may be expected
when fluticasone propionate is inhaled. Systemic corticosteroid effects
including Cushing’s syndrome and adrenal suppression have been
reported in patients receiving ritonavir and inhaled or intranasally
administered fluticasone propionate; this could also occur with other
corticosteroids metabolized via the P450 3A pathway, e.g., budesonide.
The effects of high fluticasone systemic exposure on ritonavir plasma
levels are yet unknown. The mechanism of interaction is CYP3A4
inhibition.
Co-administration of
REYATAZ/ritonavir
and these
glucocorticoids is not
recommended unless
the potential benefit of
treatment outweighs
the risk of systemic
corticosteroid effects
(see section 4.4). A
dose reduction of the
glucocorticoid should
be considered with
close monitoring of
local and systemic
effects or a switch to a
glucocorticoid, which
is not a substrate for
CYP3A4 (e.g.,
beclomethasone).
Moreover, in case of
withdrawal of
glucocorticoids,
progressive dose
reduction may have to
be performed over a
longer period.
Sildenafil, tadalafil, vardenafil Sildenafil, tadalafil, and vardenafil are metabolised by CYP3A4.
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of the PDE5 inhibitor and an increase in
PDE5-associated adverse events, including hypotension, visual changes,
Patients should be
warned about these
possible side effects
when using PDE5











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
and priapism. The mechanism of this interaction is CYP3A4 inhibition.
inhibitors for erectile
dysfunction with
REYATAZ/ritonavir
(see section 4.4).
Also see
PULMONARY
ATERIAL
HYPERTENSION in
this table for futher
information regarding
co-administration of
REYATAZ/ritonavir
with sildenafil.
St. John’s wort (Hypericum
perforatum):
Concomitant use of St. John's wort with REYATAZ/ritonavir may be
expected to result in significant reduction in plasma levels of atazanavir.
This effect may be due to an induction of CYP3A4. There is a risk of
loss of therapeutic effect and development of resistance (see section
4.3).
Co-administration of
REYATAZ/ritonavir
with products
containing St. John's
wort is contraindicated.
Ethinyloestradiol 25 μg +
norgestimate (atazanavir 300
mg QD with ritonavir 100 mg
QD)
If an oral contraceptive
is administered with
REYATAZ/ritonavir, it
is recommended that
the oral contraceptive
contain at least 30 μg
of ethinyloestradiol
and that the patient be
reminded of strict
compliance with this
contraceptive dosing
regimen. Co-
administration of
REYATAZ/ritonavir
with other hormonal
contraceptives or oral
contraceptives
containing
progestogens other
than norgestimate has
not been studied, and
therefore should be
avoided. An alternate
reliable method of
contraception is
recommended.
↑2.02
(1.77, 2.31)
While the concentration of ethinyloestradiol was increased with
atazanavir given alone, due to both UGT and CYP3A4 inhibition by
atazanavir, the net effect of atazanavir/ritonavir is a decrease in
ethinyloestradiol levels because of the inducing effect of ritonavir.
The increase in progestin exposure may lead to related side-effects (e.g.
insulin resistance, dyslipidemia, acne and spotting), thus possibly
affecting the compliance.
LIPID LOWERING AGENTS
HMG-CoA reductase inhibitors
Simvastatin
Lovastatin
Simvastatin and lovastatin are highly dependent on CYP3A4 for their
metabolism and co-administration with REYATAZ/ritonavir may result
in increased concentrations.
Co-administration of
simvastatin or
lovastatin with
REYATAZ/ritonavir is
not recommended due
to an increased risk of
myopathy including
rhabdomyolysis. The
use of another HMG-
CoA reductase
inhibitor which does
not undergo
metabolism by CYP3A
such as pravastatin or
fluvastatin is








Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
The risk of myopathy including rhabdomyolysis may also be increased
with atorvastatin, which is also metabolised by CYP3A4.
Caution should be
exercised.
INHALED BETA AGONISTS
Salmeterol
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of salmeterol and an increase in salmeterol-associated
adverse events.
Co-administration of
salmeterol with
REYATAZ/ritonavir is
not recommended (see
section 4.4).
The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Buprenorphine, QD, stable
maintenance dose,
(atazanavir 300 mg QD with
ritonavir 100 mg QD)
Co-administration
warrants
clinical monitoring for
sedation and cognitive
effects. A dose
reduction of
buprenorphine may be
considered
norbuprenorphine ↑2.05 ↑1.61 ↑2.01
The mechanism of interaction is CYP3A4 and UGT1A1 inhibition.
Concentrations of atazanavir were not significantly affected.
Methadone, stable maintenance
dose
(atazanavir 400 mg QD)
No significant effect on methadone concentrations was observed. Given
that low dose ritonavir (100 mg twice daily) has been shown to have no
significant effect on methadone concentrations, no interaction is
expected if methadone is co-administered with REYATAZ and
ritonavir, based on these data.
No dosage adjustment
is necessary if
methadone is
co-administered with
REYATAZ and
ritonavir.
PULMONARY ARTERIAL HYPERTENSION
PDE5 Inhibitors
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of the PDE5 inhibitor and an increase in PDE5-inhibitor-
associated adverse events.
A safe and effective
dose in combination
with
REYATAZ/ritonavir
has not been
established for
sildenafil when used to
treat pulmonary arterial
hypertension.
Sildenafil, when used
for the treatment of
pulmonary arterial
hypertension, is
contraindicated (see
section 4.3).
The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Midazolam and triazolam are extensively metabolized by CYP3A4.
Co-administration with REYATAZ/ritonavir may cause a large increase
in the concentration of these benzodiazepines. No drug interaction study
has been performed for the co-administration of REYATAZ/ritonavir
with benzodiazepines. Based on data for other CYP3A4 inhibitors,
plasma concentrations of midazolam are expected to be significantly
higher when midazolam is given orally. Data from concomitant use of
parenteral midazolam with other protease inhibitors suggest a possible
3-4 fold increase in midazolam plasma levels.
REYATAZ/ritonavir
should not be
co-administered with
triazolam or orally
administered
midazolam (see section
4.3), whereas caution
should be used with
co-administration of
REYATAZ/ritonavir
and parenteral
midazolam. If
REYATAZ is
co-administered with
parenteral midazolam,
it should be done in an
intensive care unit
(ICU) or similar setting
which ensures close
clinical monitoring and
appropriate medical













Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
management in case of
respiratory depression
and/or prolonged
sedation. Dosage
adjustment for
midazolam should be
considered, especially
if more than a single
dose of midazolam is
administered.
4.6 Pregnancy and lactation
There are no adequate data from the use of atazanavir in pregnant women. Studies in animals have not
shown evidence of selective developmental toxicity or effects on reproductive function and fertility
(see section 5.3). REYATAZ should be used during pregnancy only if the potential benefit justifies the
potential risk.
It is not known whether REYATAZ administered to the mother during pregnancy will exacerbate
physiological hyperbilirubinaemia and lead to kernicterus in neonates and infants. In the prepartum
period, additional monitoring and alternative therapy to REYATAZ should be considered.
It is not known whether atazanavir is excreted in human milk. Studies in rats have demonstrated that
atazanavir is excreted in the milk. It is therefore recommended that mothers being treated with
REYATAZ not breast-feed their infants. As a general rule, it is recommended that HIV infected
women not breast-feed their infants in order to avoid transmission of HIV.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. Patients
should be informed that dizziness has been reported during treatment with regimens containing
REYATAZ (see section 4.8).
REYATAZ has been evaluated for safety in combination therapy with other antiretroviral medicinal
products in controlled clinical trials in 1,806 adult patients receiving REYATAZ 400 mg once daily
(1,151 patients, 52 weeks median duration and 152 weeks maximum duration) or REYATAZ 300 mg
with ritonavir 100 mg once daily (655 patients, 96°weeks median duration and 108 weeks maximum
duration).
Adverse reactions were consistent between patients who received REYATAZ 400 mg once daily and
patients who received REYATAZ 300 mg with ritonavir 100 mg once daily, except that jaundice and
elevated total bilirubin levels were reported more frequently with REYATAZ plus ritonavir.
Among patients who received REYATAZ 400 mg once daily or REYATAZ 300 mg with ritonavir
100 mg once daily, the only adverse reactions of any severity reported very commonly with at least a
possible relationship to
regimens containing REYATAZ and one or more NRTIs were nausea (20%),
diarrhoea (10%), and jaundice (13%). Among patients receiving REYATAZ 300 mg with ritonavir
100 mg, the frequency of jaundice was 19%. In the majority of cases, jaundice was reported within a
few days to a few months after the initiation of treatment (see section 4.4).
Combination antiretroviral therapy has been associated with redistribution of body fat (lipodystrophy)
in HIV patients, including loss of peripheral and facial subcutaneous fat, increased intra-abdominal
and visceral fat, breast hypertrophy, and dorsocervical fat accumulation (buffalo hump).


Combination antiretroviral therapy has been associated with metabolic abnormalities such as
hypertriglyceridaemia, hypercholesterolaemia, insulin resistance, hyperglycaemia, and
hyperlactataemia (see sections 4.4 and 5.1).
Adult patients
The following adverse reactions of moderate intensity or greater with at least a possible relationship to
regimens containing REYATAZ and one or more NRTIs have also been reported. The frequency of
adverse reactions listed below is defined using the following convention: very common (≥ 1/10),
common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), or
very rare (< 1/10,000). Within each frequency grouping, undesirable effects are presented in order of
decreasing seriousness.
rare: oedema, palpitation
Nervous system disorders:
common: headache;
uncommon: peripheral neuropathy, syncope, amnesia,
dizziness, somnolence, dysgeusia
Respiratory, thoracic and
mediastinal disorders:
Gastrointestinal disorders:
common: vomiting, diarrhoea, abdominal pain, nausea,
dyspepsia;
uncommon: pancreatitis, gastritis, abdominal distension,
stomatitis aphthous, flatulence, dry mouth
Renal and urinary disorders:
uncommon: nephrolithiasis, hematuria, proteinuria,
pollakiuria;
rare: kidney pain
Skin and subcutaneous tissue
disorders:
common: rash;
uncommon: urticaria, alopecia, pruritus;
rare: vesiculobullous rash, eczema, vasodilatation
Musculoskeletal and connective
tissue disorders:
uncommon: muscle atrophy, arthralgia, myalgia;
rare: myopathy
Metabolism and nutrition
disorders:
uncommon: weight decreased, weight gain, anorexia,
appetite increased
General disorders and
administration site conditions:
common: lipodystrophy syndrome, fatigue;
uncommon: chest pain, malaise, pyrexia, asthenia;
rare: gait disturbance
uncommon: hypersensitivity
common: jaundice;
uncommon: hepatitis;
rare: hepatosplenomegaly
Reproductive system and breast
disorders:
uncommon: depression, disorientation, anxiety, insomnia,
sleep disorder, abnormal dream
In HIV-infected patients with severe immune deficiency at the time of initiation of combination
antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic
infections may arise (see section 4.4).
Cases of osteonecrosis have been reported, particularly in patients with generally acknowledged risk
factors, advanced HIV disease or long-term exposure to combination antiretroviral therapy (CART).
The frequency of this is unknown (see section 4.4).
Laboratory abnormalities
The most frequently reported laboratory abnormality in patients receiving regimens containing
REYATAZ and one or more NRTIs was elevated total bilirubin reported predominantly as elevated
indirect [unconjugated] bilirubin (87% Grade 1, 2, 3, or 4). Grade 3 or 4 elevation of total bilirubin
was noted in 37% (6% Grade 4). Among experienced patients treated with REYATAZ 300 mg once
daily with 100 mg ritonavir once daily for a median duration of 95 weeks, 53% had Grade 3-4 total
bilirubin elevations. Among naive patients treated with REYATAZ 300 mg once daily with 100 mg
ritonavir once daily for a median duration of 96 weeks, 48% had Grade 3-4 total bilirubin elevations
(see section 4.4).
Other marked clinical laboratory abnormalities (Grade 3 or 4) reported in ≥ 2% of patients receiving
regimens containing REYATAZ and one or more NRTIs included: elevated creatine kinase (7%),
elevated alanine aminotransferase/serum glutamic-pyruvic transaminase (ALT/SGPT) (5%), low
neutrophils (5%), elevated aspartate aminotransferase/serum glutamic-oxaloacetic transaminase
(AST/SGOT) (3%), and elevated lipase (3%).
Two percent of patients treated with REYATAZ experienced concurrent Grade 3-4 ALT/AST and
Grade 3-4 total bilirubin elevations.
Patients co-infected with hepatitis B and/or hepatitis C virus
Among 1,151 patients receiving atazanavir 400 mg once daily, 177 patients were co-infected with
chronic hepatitis B or C, and among 655 patients receiving atazanavir 300 mg once daily with
ritonavir 100 mg once daily, 97 patients were co-infected with chronic hepatitis B or C. Co-infected
patients were more likely to have baseline hepatic transaminase elevations than those without chronic
viral hepatitis. No differences in frequency of bilirubin elevations were observed between these
patients and those without viral hepatitis. The frequency of treatment emergent hepatitis or
transaminase elevations in co-infected patients was comparable between REYATAZ and comparator
regimens (see section 4.4).
Paediatric population
In clinical studies, paediatric patients 3 months to less than 18 years of age had a mean duration of
treatment with REYATAZ of 115 weeks. The safety profile in these studies was overall comparable to
that seen in adults. Both asymptomatic first-degree (23%) and second-degree (1%) atrioventricular
block were reported in paediatric patients. The most frequently reported laboratory abnormality in
paediatric patients receiving REYATAZ was elevation of total bilirubin (≥ 2.6 times ULN , Grade 3-4)
which occurred in 45% of patients.
Postmarketing experience
There have been postmarketing reports of unknown frequency for torsades de pointes, QTc
prolongation, diabetes mellitus, hyperglycaemia, nephrolithiasis, and gallbladder disorders including
cholelithiasis, cholecystitis, and cholestasis.
Human experience of acute overdose with REYATAZ is limited. Single doses up to 1,200 mg have
been taken by healthy volunteers without symptomatic untoward effects. At high doses that lead to
high drug exposures, jaundice due to indirect (unconjugated) hyperbilirubinaemia (without associated
liver function test changes) or PR interval prolongations may be observed (see sections 4.4 and 4.8).
Treatment of overdose with REYATAZ should consist of general supportive measures, including
monitoring of vital signs and electrocardiogram (ECG), and observations of the patient's clinical
status. If indicated, elimination of unabsorbed atazanavir should be achieved by emesis or gastric
lavage. Administration of activated charcoal may also be used to aid removal of unabsorbed drug.
There is no specific antidote for overdose with REYATAZ. Since atazanavir is extensively
metabolised by the liver and is highly protein bound, dialysis is unlikely to be beneficial in significant
removal of this medicinal product.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: protease inhibitor, ATC code: J05AE08
Mechanism of action:
atazanavir is an azapeptide HIV-1 protease inhibitor (PI). The compound
selectively inhibits the virus-specific processing of viral Gag-Pol proteins in HIV-1 infected cells, thus
preventing formation of mature virions and infection of other cells.
Antiviral activity
in vitro:
atazanavir exhibits anti-HIV-1 (including all clades tested) and anti-HIV-2
activity in cell culture.
Resistance
Antiretroviral treatment naive adult patients
In clinical trials of antiretroviral treatment naive patients treated with unboosted atazanavir, the I50L
substitution, sometimes in combination with an A71V change, is the signature resistance substitution
for atazanavir. Resistance levels to atazanavir ranged from 3.5- to 29-fold without evidence of
phenotypic cross resistance to other PIs. In clinical trials of antiretroviral treatment naive patients
treated with boosted atazanavir, the I50L substitution did not emerge in any patient without baseline PI
substitutions. The N88S substitution has been rarely observed in patients with virologic failure on
atazanavir (with or without ritonavir). While it may contribute to decreased susceptibility to atazanavir
when it occurs with other protease substitutions, in clinical studies N88S by itself does not always lead
to phenotypic resistance to atazanavir or have a consistent impact on clinical efficacy.
Table 3. De novo substitutions in treatment naive patients failing therapy with atazanavir +
ritonavir (Study 138, 96 weeks)
Frequency de novo PI substitution (n=26)
a
>20% none
10-20% none
a
Number of patients with paired genotypes classified as virological failures (HIV RNA ≥ 400 copies/ml).
The M184I/V substitution emerged in 5/26 REYATAZ/ritonavir and 7/26 lopinavir/ritonavir virologic
failure patients, respectively.
Antiretroviral treatment experienced adult patients
In antiretroviral treatment experienced patients from Studies 009, 043, and 045, 100 isolates from
patients designated as virological failures on therapy that included either atazanavir, atazanavir +
ritonavir, or atazanavir + saquinavir were determined to have developed resistance to atazanavir. Of
the 60 isolates from patients treated with either atazanavir or atazanavir + ritonavir, 18 (30%)
displayed the I50L phenotype previously described in naive patients.
Table 4. De novo substitutions in treatment experienced patients failing therapy with atazanavir
+ ritonavir (Study 045, 48 weeks)
Frequency
de novo PI substitution (n=35)
a,b




>20% M36, M46, I54, A71, V82
10-20% L10, I15, K20, V32, E35, S37, F53, I62, G73, I84, L90
a
Number of patients with paired genotypes classified as virological failures (HIV RNA ≥ 400 copies/ml).
b
Ten patients had baseline phenotypic resistance to atazanavir + ritonavir (fold change [FC]>5.2). FC susceptibility in cell
culture relative to the wild-type reference was assayed using PhenoSense
TM
(Monogram Biosciences, South San Francisco,
California, USA)
None of the de novo substitutions (see Table 4) are specific to atazanavir and may reflect re-
emergence of archived resistance on atazanavir + ritonavir in Study 045 treatment-experienced
population.
The resistance in antiretroviral treatment experienced patients mainly occurs by accumulation of the
major and minor resistance substitutions described previously to be involved in protease inhibitor
resistance.
Clinical results
In antiretroviral naive adult patients
Study 138
is an international randomised, open-label, multicenter, prospective trial of treatment naïve
patients comparing REYATAZ/ritonavir (300 mg/100 mg once daily) to lopinavir/ritonavir
(400 mg/100 mg twice daily), each in combination with fixed dose tenofovir/emtricitabine
(300 mg/200 mg tablets once daily). The REYATAZ/ritonavir arm showed similar (non-inferior)
antiviral efficacy compared to the lopinavir/ritonavir arm, as assessed by the proportion of patients
with HIV RNA < 50 copies/ml at week 48 (Table 5).
Analyses of data through 96 weeks of treatment demonstrated durability of antiviral activity (Table 5).

Table 5: Efficacy Outcomes in Study 138
a
REYATAZ/ritonavir
b
(300 mg/100 mg once daily)
n=440
Lopinavir/ritonavir
c
(400 mg/100 mg twice daily)
n=443
HIV RNA <50 copies/ml, %
All patients
d
Difference estimate
[95% CI]
d
Week 48: 1.7% [-3.8%, 7.1%]
Week 96: 6.1% [0.3%, 12.0%]
Week 48: -3% [-7.6%, 1.5%]
Week 96: 2.2% [-2.3%, 6.7%]
HIV RNA <50 copies/ml, % by Baseline Characteristic
d
HIV RNA
<100,000 copies/ml
HIV RNA Mean Change from Baseline, log
10
copies/ml
All patients
CD4 Mean Change from Baseline, cells/mm
3
All patients
CD4 Mean Change from Baseline, cells/mm
3
by Baseline Characteristic
HIV RNA
<100,000 copies/ml
≥100,000 copies/ml 227 (n=187) 291 (n=173) 245 (n=180) 310 (n=165)
a
Mean baseline CD4 cell count was 214 cells/mm
3
(range 2 to 810 cells/mm
3
) and mean baseline plasma HIV-1 RNA was
4.94 log
10
copies/ml (range 2.6 to 5.88 log
10
copies/ml)
b
REYATAZ/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
c
Lopinavir/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
d
Intent-to-treat analysis, with missing values considered as failures.
e
Per protocol analysis: Excluding non-completers and patients with major protocol deviations.
f
Number of patients evaluable.
In antiretroviral experienced adult patients
Study 045
is a randomised, multicenter trial comparing REYATAZ/ritonavir (300/100 mg once daily)
and REYATAZ/saquinavir (400/1,200 mg once daily), to lopinavir + ritonavir (400/100 mg fixed dose
combination twice daily), each in combination with tenofovir (see sections 4.5 and 4.8) and one NRTI,
in patients with virologic failure on two or more prior regimens containing at least one PI, NRTI, and
NNRTI. For randomised patients, the mean time of prior antiretroviral exposure was 138 weeks for
PIs, 281 weeks for NRTIs, and 85 weeks for NNRTIs. At baseline, 34% of patients were receiving a
PI and 60% were receiving an NNRTI. Fifteen of 120 (13%) patients in the REYATAZ + ritonavir
treatment arm and 17 of 123 (14%) patients in the lopinavir + ritonavir arm had four or more of the PI
substitutions L10, M46, I54, V82, I84, and L90. Thirty-two percent of patients in the study had a viral
strain with fewer than two NRTI substitutions.
The primary endpoint was the time-averaged difference in change from baseline in HIV RNA through
48 weeks (Table 6).
Difference estimate
e
[95% CI]
























Table 6: Efficacy Outcomes at Week 48
a
and at Week 96 (Study 045)
ATV/RTV
b
(300 mg/
100 mg once daily)
n=120
LPV/RTV
c
(400 mg/
100 mg twice daily)
n=123
Time-averaged difference
ATV/RTV-LPV/RTV
[97.5% CI
d
]
HIV RNA Mean Change from Baseline, log
10
copies/ml
All patients
HIV RNA <50 copies/ml, %
f
(responder/evaluable)
All patients
36 (43/120) 32 (38/120) 42 (52/123 35 (41/118)
HIV RNA <50 copies/ml by select baseline PI substitutions,
f, g
% (responder/evaluable)
0-2
CD4 Mean Change from Baseline, cells/mm
3
All patients 110 (n=83) 122 (n=60) 121 (n=94) 154 (n=60) NA NA
a
The mean baseline CD4 cell count was 337 cells/mm
3
(range: 14 to 1,543 cells/mm
3
) and the mean baseline plasma HIV-1
RNA level was 4.4 log
10
copies/ml (range: 2.6 to 5.88 log
10
copies/ml).
b
ATV/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
c
LPV/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
d
Confidence interval.
e
Number of patients evaluable.
f
Intent-to-treat analysis, with missing values considered as failures. Responders on LPV/RTV who completed treatment
before Week 96 are excluded from Week 96 analysis. The proportion of patients with HIV RNA < 400 copies/ml were 53%
and 43% for ATV/RTV and 54% and 46% for LPV/RTV at weeks 48 and 96 respectively.
g
Select substitutions include any change at positions L10, K20, L24, V32, L33, M36, M46, G48, I50, I54, L63, A71, G73,
V82, I84, and L90 (0-2, 3, 4 or more) at baseline.
NA = not applicable.
Through 48 weeks of treatment, the mean changes from baseline in HIV RNA levels for REYATAZ +
ritonavir and lopinavir + ritonavir were similar (non-inferior). Consistent results were obtained with
the last observation carried forward method of analysis (time-averaged difference of 0.11, 97.5%
confidence interval [-0.15, 0.36]). By as-treated analysis, excluding missing values, the proportions of
patients with HIV RNA < 400 copies/ml (< 50 copies/ml) in the REYATAZ + ritonavir arm and the
lopinavir + ritonavir arm were 55% (40%) and 56% (46%), respectively.
Through 96 weeks of treatment, mean HIV RNA changes from baseline for REYATAZ + ritonavir
and lopinavir + ritonavir met criteria for non-inferiority based on observed cases. Consistent results
were obtained with the last observation carried forward method of analysis. By as-treated analysis,
excluding missing values, the proportions of patients with HIV RNA <400 copies/ml (<50 copies/ml)
for REYATAZ + ritonavir were 84% (72%) and for lopinavir + ritonavir were 82% (72%). It is
important to note that at time of the 96-week analysis, 48 % of patients overall remained on study.
REYATAZ + saquinavir was shown to be inferior to lopinavir + ritonavir.
Paediatric population
Assessment of the pharmacokinetics, safety, tolerability, and efficacy of REYATAZ is based on data
from the open-label, multicenter clinical trial PACTG 1020A conducted in patients from 3 months to
21 years of age. Overall in this study, 182 paediatric patients (81 antiretroviral-naive and
101 antiretroviral-experienced) received once daily REYATAZ (capsule or powder formulation), with
or without ritonavir, in combination with two NRTIs.
The clinical data derived from this study are inadequate to support the use of atazanavir (with or
without ritonavir) in children below 6 years of age.
Efficacy data observed in the 41 paediatric patients aged 6 years to less than 18 years that received
REYATAZ capsules with ritonavir are presented in Table 7. For treatment-naive paediatric patients,
the mean baseline CD4 cell count was 344 cells/mm
3
(range: 2 to 800 cells/ mm
3
) and mean baseline
















plasma HIV 1 RNA was 4.67 log
10
copies/ml (range: 3.70 to 5.00 log
10
copies/ml). For treatment-
experienced paediatric patients, the mean baseline CD4 cell count was 522 cells/mm
3
(range: 100 to
1157 cells/ mm
3
) and mean baseline plasma HIV 1 RNA was 4.09 log
10
copies/ml (range: 3.28 to
5.00 log
10
copies/ml).
Table 7: Efficacy Outcomes (paediatric patients 6 years to less than 18 years of age) at Week
48 (Study PACTG 1020A)
Treatment-Naive
REYATAZ
Capsules/ritonavir
(300 mg/100 mg once
daily) n=16
Treatment-
Experienced
REYATAZ
Capsules/ritonavir
(300 mg/100 mg once
daily) n=25
HIV RNA <50 copies/ml, %
a
All patients
HIV RNA <400 copies/ml, %
a
All patients
CD4 Mean Change from Baseline, cells/mm
3
All patients 293 (n=14
b
)
229 (n=14
b
)
HIV RNA <50 copies/ml by select baseline PI substitutions,
c
% (
responder/evaluable
d
)
0-2
a
Intent-to-treat analysis, with missing values considered as failures.
b
Number of patients evaluable.
c
PI major L24I, D30N, V32I, L33F, M46IL, I47AV, G48V, I50LV, F53LY,I54ALMSTV, L76V, V82AFLST,
I84V, N88DS, L90M; PI minor: L10CFIRV, V11I, E35G, K43T, Q58E, A71ILTV, G73ACST, T74P, N83D,
L89V.
d
Includes patients with baseline resistance data.
NA = not applicable.
Data in the paediatric population are very limited. Available data do suggest that atazanavir in
combination with ritonavir may not be effective in treatment experienced children even with very few
(<3) PI mutations.
5.2 Pharmacokinetic properties
The pharmacokinetics of atazanavir were evaluated in healthy adult volunteers and in HIV-infected
patients; significant differences were observed between the two groups. The pharmacokinetics of
atazanavir exhibit a non-linear disposition. In healthy subjects, the AUC of atazanavir from the capsules
and oral powder were similar.
Absorption:
in HIV-infected patients (n=33, combined studies), multiple dosing of REYATAZ 300 mg
once daily with ritonavir 100 mg once daily with food produced a geometric mean (CV%) for
atazanavir, C
max
of 4466 (42%) ng/ml, with time to C
max
of approximately 2.5 hours. The geometric
mean (CV%) for atazanavir C
min
and AUC was 654 (76%) ng/ml and 44185 (51%) ng•h/ml,
respectively.
Food effect:
co-administration of REYATAZ and ritonavir with food optimises the bioavailability of
atazanavir. Co-administration of a single 300-mg dose of REYATAZ and 100-mg dose of ritonavir
with a light meal resulted in a 33% increase in the AUC and a 40% increase in both the C
max
and the
24-hour concentration of atazanavir relative to the fasting state. Co-administration with a high-fat meal
did not affect the AUC of atazanavir relative to fasting conditions and the C
max
was within 11% of
fasting values. The 24-hour concentration following a high fat meal was increased by approximately
33% due to delayed absorption; the median T
max
increased from 2.0 to 5.0 hours. Administration of
REYATAZ with ritonavir with either a light or a high-fat meal decreased the coefficient of variation

























of AUC and C
max
by approximately 25% compared to the fasting state. To enhance bioavailability and
minimise variability, REYATAZ is to be taken with food.
Distribution:
atazanavir was approximately 86% bound to human serum proteins over a concentration
range of 100 to 10,000 ng/ml. Atazanavir binds to both alpha-1-acid glycoprotein (AAG) and albumin
to a similar extent (89% and 86%, respectively, at 1,000 ng/ml). In a multiple-dose study in
HIV-infected patients dosed with 400 mg of atazanavir once daily with a light meal for 12 weeks,
atazanavir was detected in the cerebrospinal fluid and semen.
Metabolism:
studies in humans and
in vitro
studies using human liver microsomes have demonstrated
that atazanavir is principally metabolised by CYP3A4 isozyme to oxygenated metabolites.
Metabolites
are then excreted in the bile as either free or glucuronidated metabolites. Additional minor metabolic
pathways consist of N-dealkylation and hydrolysis. Two minor metabolites of atazanavir in plasma
have been characterised. Neither metabolite demonstrated
in vitro
antiviral activity.
Elimination:
following a single 400-mg dose of
14
C-atazanavir, 79% and 13% of the total radioactivity
was recovered in the faeces and urine, respectively. Unchanged drug accounted for approximately
20% and 7% of the administered dose in the faeces and urine, respectively. Mean urinary excretion of
unchanged drug was 7% following 2 weeks of dosing at 800 mg once daily. In HIV-infected adult
patients (n=33, combined studies) the mean half-life within a dosing interval for atazanavir was 12
hours at steady state following a dose of 300 mg daily with ritonavir 100 mg once daily with a light
meal.
Paediatric patients:
The pharmacokinetics of atazanavir in paediatric patients exhibit an increased
absorption rate compared to adults. There is a slight trend toward a higher clearance in younger
children when normalised for body weight. As a result, greater peak to trough ratios are observed. The
geometric mean AUC values in paediatric patients at recommended doses are expected to be similar to
those observed in adults, with higher geometric mean C
max
(13-17%) and lower geometric mean C
min
(up to 30%) values compared to those in adults. The variability of pharmacokinetic parameters in
younger children is higher.
Impaired renal function
: in healthy subjects, the renal elimination of unchanged atazanavir was
approximately 7% of the administered dose. There are no pharmacokinetic data available for
REYATAZ with ritonavir in patients with renal insufficiency. REYATAZ (without ritonavir) has been
studied in adult patients with severe renal impairment (n=20), including those on haemodialysis, at
multiple doses of 400 mg once daily. Although this study presented some limitations (i.e., unbound
drug concentrations not studied), results suggested that the atazanavir pharmacokinetic parameters
were decreased by 30% to 50% in patients undergoing haemodialysis compared to patients with
normal renal function. The mechanism of this decrease is unknown. (See sections 4.2 and 4.4.)
Impaired hepatic function
: atazanavir is metabolised and eliminated primarily by the liver. The effects
of hepatic impairment on the pharmacokinetics of atazanavir after a 300 mg dose with ritonavir have
not been studied. Concentrations of atazanavir with or without ritonavir are expected to be increased in
patients with moderately or severely impaired hepatic function (see sections 4.2, 4.3, and 4.4).
Age/Gender:
a study of the pharmacokinetics of atazanavir was performed in 59 healthy male and
female subjects (29 young, 30 elderly). There were no clinically important pharmacokinetic
differences based on age or gender.
Race:
a population pharmacokinetic analysis of samples from Phase II clinical trials indicated no
effect of race on the pharmacokinetics of atazanavir.
5.3 Preclinical safety data
In repeat-dose toxicity studies, conducted in mice, rats, and dogs, atazanavir-related findings were
generally confined to the liver and included generally minimal to mild increases in serum bilirubin and
liver enzymes, hepatocellular vacuolation and hypertrophy, and, in female mice only, hepatic
single-cell necrosis. Systemic exposures of atazanavir in mice (males), rats, and dogs at doses
associated with hepatic changes were at least equal to that observed in humans given 400 mg once
daily. In female mice, atazanavir exposure at a dose that produced single-cell necrosis was 12 times
the exposure in humans given 400 mg once daily. Serum cholesterol and glucose were minimally to
mildly increased in rats but not in mice or dogs.
During in vitro studies, cloned human cardiac potassium channel (hERG), was inhibited by 15% at a
concentration (30 μM) of atazanavir corresponding to 30-fold the free drug concentration at C
max
in
humans. Similar concentrations of atazanavir increased by 13% the action potential duration (APD
90
)
in rabbit Purkinje fibres study. Electrocardiographic changes (sinus bradycardia, prolongation of PR
interval, prolongation of QT interval, and prolongation of QRS complex) were observed only in an
initial 2-week oral toxicity study performed in dogs. Subsequent 9-month oral toxicity studies in dogs
showed no drug-related electrocardiographic changes. The clinical relevance of these non-clinical data
is unknown. Potential cardiac effects of this product in humans cannot be ruled out (see sections 4.4
and 4.8). The potential for PR prolongation should be considered in cases of overdose (see section4.9).
In a fertility and early embryonic development study in rats, atazanavir altered oestrus cycling with no
effects on mating or fertility. No teratogenic effects were observed in rats or rabbits at maternally toxic
doses. In pregnant rabbits, gross lesions of the stomach and intestines were observed in dead or
moribund does at maternal doses 2 and 4 times the highest dose administered in the definitive
embryo-development study. In the pre- and postnatal development assessment in rats, atazanavir
produced a transient reduction in body weight in the offspring at a maternally toxic dose. Systemic
exposure to atazanavir at doses that resulted in maternal toxicity was at least equal to or slightly
greater than that observed in humans given 400 mg once daily.
Atazanavir was negative in an Ames reverse-mutation assay but did induce chromosomal aberrations
in vitro
in both the absence and presence of metabolic activation. In
in vivo
studies in rats, atazanavir
did not induce micronuclei in bone marrow, DNA damage in duodenum (comet assay), or unscheduled
DNA repair in liver at plasma and tissue concentrations exceeding those that were clastogenic
in vitro
.
In long-term carcinogenicity studies of atazanavir in mice and rats, an increased incidence of benign
hepatic adenomas was seen in female mice only. The increased incidence of benign hepatic adenomas
in female mice was likely secondary to cytotoxic liver changes manifested by single-cell necrosis and
is considered to have no relevance for humans at intended therapeutic exposures. There were no
tumorigenic findings in male mice or in rats.
Atazanavir increased opacity of bovine corneas in an
in vitro
ocular irritation study, indicating it may
be an ocular irritant upon direct contact with the eye.
PHARMACEUTICAL PARTICULARS
Capsule contents:
Crospovidone
Lactose monohydrate
Magnesium stearate
Capsule shells:
Gelatine
Indigocarmin (E132)
Blue ink containing:
Shellac
Propylene glycol
Ammonium hydroxide
Indigocarmin (E132)
White ink containing:
Shellac
Titanium dioxide (E171)
Ammonium hydroxide
Propylene glycol
Simethicone
6.4 Special precautions for storage
6.5 Nature and contents of container
Each carton contains one high-density polyethylene (HDPE) bottle closed with child-resistant
polypropylene closure. Each bottle contains 60 hard capsules.
Each carton contains 60 x 1 capsules; 10 blister cards of 6 x 1 capsules each in Alu/Alu perforated unit
dose blisters.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
Any unused product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
BRISTOL-MYERS SQUIBB PHARMA EEIG
Uxbridge Business Park
Sanderson Road
Uxbridge UB8 1DH
United Kingdom
MARKETING AUTHORISATION NUMBER(S)
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 02 March 2004
Date of latest renewal: 02 March 2009
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency (EMEA) http://www.emea.europa.eu
NAME OF THE MEDICINAL PRODUCT
REYATAZ 150 mg hard capsules
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each capsule contains 150 mg of atazanavir (as sulphate)
Excipient: 82.18 mg of lactose per capsule.
For a full list of excipients, see section 6.1.
Hard capsule
Opaque blue and powder blue capsule printed with white and blue inks, with "BMS 150 mg" on one
half and with "3624" on the other half.
4.1 Therapeutic indications
REYATAZ capsules, co-administered with low dose ritonavir, are indicated for the treatment of
HIV-1 infected adults and paediatric patients 6 years of age and older in combination with other
antiretroviral medicinal products.
Based on available virological and clinical data from adult patients, no benefit is expected in patients
with strains resistant to multiple protease inhibitors (
The choice of REYATAZ in treatment experienced adult and paediatric patients should be based on
individual viral resistance testing and the patient’s treatment history (see sections 4.4 and 5.1).
4.2 Posology and method of administration
Therapy should be initiated by a physician experienced in the management of HIV infection.
Adults:
the recommended dose of REYATAZ capsules is 300 mg once daily taken with ritonavir
100 mg once daily and with food. Ritonavir is used as a booster of atazanavir pharmacokinetics
(see sections 4.5 and 5.1).
Paediatric patients (6 years to less than 18 years of age):
The dose of REYATAZ capsules for
paediatric patients is based on body weight as shown in Table 1 and should not exceed the
recommended adult dose. REYATAZ capsules must be taken with ritonavir and have to be taken with
food.
4 PI mutations). There are very limited data
available from children aged 6 to less than 18 years (see sections 4.4 and 5.1).
Table 1: Dose for Paediatric Patients (6 years to less than 18 years of age) for REYATAZ
capsules with ritonavir
Body Weight (kg)
a
Ritonavir capsules, tablets or oral solution.
b
Ritonavir oral solution no lower than 80 mg and not more than 100 mg may be used for paediatric
patients from 15 kg to less than 20 kg who cannot swallow ritonavir capsules/tablets.
The available data do not support the use of REYATAZ in combination with low dose ritonavir in
paediatric patients weighing less than 15 kg.
Paediatric patients (less than 6 years of age):
REYAYAZ is not recommended in paediatric patients
less than 6 years of age due to insufficient data on pharmacokinetics, safety, and efficacy. REYATAZ
has not been studied in children less than 3 months of age and is not recommended especially taking
into account the potential risk of kernicterus.
Patients with renal impairment:
no dosage adjustment is needed. REYATAZ with ritonavir is not
recommended in patients undergoing haemodialysis (see sections 4.4 and 5.2).
Patients with hepatic impairment:
REYATAZ with ritonavir has not been studied in patients with
hepatic impairment. REYATAZ with ritonavir should be used with caution in patients with mild
hepatic impairment. REYATAZ must not be used in patients with moderate to severe hepatic
impairment (see sections 4.3, 4.4, and 5.2).
Method of administration
: for oral administration. The capsules should be swallowed whole.
REYATAZ oral powder is available for adult patients who are unable to swallow capsules
(see Summary of Product Characteristics for REYATAZ oral powder). REYATAZ oral powder must
not be used in paediatric patients unable to swallow capsules due to insufficient data on
pharmacokinetics, safety, and efficacy.
Hypersensitivity to the active substance or to any of the excipients (see section 6.1).
Patients with moderate to severe hepatic insufficiency (see sections 4.2 and 4.4).
Combination of rifampicin and REYATAZ with concomitant low-dose ritonavir is contraindicated
(see section 4.5).
The PDE5 inhibitor sildenafil is contraindicated when used for the treatment of pulmonary arterial
hypertension (PAH) only (see section 4.5). For co-administration of sildenafil for the treatment of
erectile dysfunction see section 4.4 and section 4.5.
REYATAZ with ritonavir must not be used in combination with medicinal products that are substrates
of the CYP3A4 isoform of cytochrome P450 and have narrow therapeutic windows (e.g., alfuzosin,
astemizole, terfenadine, cisapride, pimozide, quinidine, bepridil, triazolam, midazolam administered
orally (for caution on parenterally administered midazolam, see section 4.5),
and ergot alkaloids,
particularly, ergotamine, dihydroergotamine, ergonovine, methylergonovine) (see section 4.5).
REYATAZ must not be used in combination with products containing St. John’s wort (
Hypericum
perforatum
) (see section 4.5).

4.4 Special warnings and precautions for use
Patients should be advised that current antiretroviral therapy has not been proven to prevent the risk of
transmission of HIV to others through blood or sexual contact. Appropriate precautions should
continue to be employed.
Co-administration of REYATAZ with ritonavir at doses greater than 100 mg once daily has not been
clinically evaluated. The use of higher ritonavir doses may alter the safety profile of atazanavir
(cardiac effects, hyperbilirubinaemia) and therefore is not recommended. Only when atazanavir with
ritonavir is co-administered with efavirenz, a dose increase of ritonavir to 200 mg once daily could be
considered. In this instance, close clinical monitoring is warranted (see Interaction with other
Medicinal Products below).
Patients with coexisting conditions
Atazanavir is primarily hepatically metabolised and increased plasma concentrations were observed in
patients with hepatic impairment
(see sections 4.2 and 4.3). The safety and efficacy of REYATAZ has
not been established in patients with significant underlying liver disorders. Patients with chronic
hepatitis B or C and treated with combination antiretroviral therapy are at an increased risk for severe
and potentially fatal hepatic adverse reactions. In case of concomitant antiviral therapy for hepatitis B
or C, please refer also to the relevant Summary of Product Characteristics for these medicinal products
(see section 4.8).
Patients with pre-existing liver dysfunction, including chronic active hepatitis, have an increased
frequency of liver function abnormalities during combination antiretroviral therapy and should be
monitored according to standard practice. If there is evidence of worsening liver disease in such
patients, interruption or discontinuation of treatment must be considered.
No dosage adjustment is needed in patients with renal impairment. However, REYATAZ with
ritonavir is not recommended in patients undergoing haemodialysis (see sections 4.2 and 5.2).
Dose related asymptomatic prolongations in PR interval with REYATAZ have been observed in
clinical studies. Caution should be used with medicinal products known to induce PR prolongations. In
patients with pre-existing conduction problems (second degree or higher atrioventricular or complex
bundle-branch block), REYATAZ should be used with caution and only if the benefits exceed the risk
(see section 5.1). Particular caution should be used when prescribing REYATAZ in association with
medicinal products which have the potential to increase the QT interval and/or in patients with
pre-existing risk factors (bradycardia, long congenital QT, electrolyte imbalances (see sections 4.8 and
5.3).
There have been reports of increased bleeding, including spontaneous skin haematomas and
haemarthroses, in type A and B haemophiliac patients treated with protease inhibitors. In some
patients additional factor VIII was given. In more than half of the reported cases, treatment with
protease inhibitors was continued or reintroduced if treatment had been discontinued. A causal
relationship has been suggested, although the mechanism of action has not been elucidated.
Haemophiliac patients should therefore be made aware of the possibility of increased bleeding.
Fat redistribution and metabolic disorders
Combination antiretroviral therapy has been associated with the redistribution of body fat
(lipodystrophy) in HIV patients. The long-term consequences of these events are currently unknown.
Knowledge about the mechanism is incomplete. A connection between visceral lipomatosis and
protease inhibitors and lipoatrophy and nucleoside reverse transcriptase inhibitors has been
hypothesised. A higher risk of lipodystrophy has been associated with individual factors such as older
age, and with drug related factors such as longer duration of antiretroviral treatment and associated
metabolic disturbances. Clinical examination should include evaluation for physical signs of fat
redistribution.
Combination antiretroviral therapy (CART), including REYATAZ (with or without ritonavir)-based
CART, is associated with dyslipidaemia. Consideration should be given to the measurement of fasting
serum lipids and blood glucose. Lipid disorders should be managed as clinically appropriate
(see section 4.8).
In clinical studies, REYATAZ (with or without ritonavir) has been shown to induce dyslipidaemia to a
lesser extent than comparators. The clinical impact of such findings has not been demonstrated in the
absence of specific studies on cardiovascular risk. The selection of antiretroviral therapy must be
guided principally by antiviral efficacy. Consultation with standard guidelines for management of
dyslipidaemia is recommended.
Hyperglycaemia
New onset diabetes mellitus, hyperglycaemia, and exacerbation of existing diabetes mellitus have been
reported in patients receiving protease inhibitors. In some of these, the hyperglycaemia was severe and
in some cases also associated with ketoacidosis. Many patients had confounding medical conditions,
some of which required therapy with medicinal products that have been associated with development
of diabetes or hyperglycaemia.
Hyperbilirubinaemia
Reversible elevations in indirect (unconjugated) bilirubin related to inhibition of UDP-glucuronosyl
transferase (UGT) have occurred in patients receiving REYATAZ (see section 4.8). Hepatic
transaminase elevations that occur with elevated bilirubin in patients receiving REYATAZ should be
evaluated for alternative etiologies. Alternative antiretroviral therapy to REYATAZ may be
considered if jaundice or scleral icterus is unacceptable to a patient. Dose reduction of atazanavir is not
recommended because it may result in a loss of therapeutic effect and development of resistance.
Indinavir is also associated with indirect (unconjugated) hyperbilirubinaemia due to inhibition of
UGT. Combinations of REYATAZ and indinavir have not been studied and co-administration of these
medicinal products is not recommended (see section 4.5).
Nephrolithiasis
Nephrolithiasis has been reported in patients receiving REYATAZ (see section 4.8). If signs or
symptoms of nephrolithiasis occur, temporary interruption or discontinuation of treatment may be
considered.
Immune reactivation syndrome
In HIV-infected patients with severe immune deficiency at the time of institution of combination
antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic
pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically,
such reactions have been observed within the first few weeks or months of initiation of CART.
Relevant examples are cytomegalovirus retinitis, generalised and/or focal mycobacterial infections,
and
Pneumocystis carinii
pneumonia. Any inflammatory symptoms should be evaluated and treatment
instituted when necessary.
Osteonecrosis
Although the etiology is considered to be multifactorial (including corticosteroid use, alcohol
consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been
reported particularly in patients with advanced HIV-disease and/or long-term exposure to combination
antiretroviral therapy (CART). Patients should be advised to seek medical advice if they experience
joint aches and pain, joint stiffness or difficulty in movement.
Interactions with other medicinal products
Co-administration of REYATAZ with simvastatin or lovastatin is not recommended (see section 4.5).
Co-administration of REYATAZ with nevirapine or efavirenz is not recommended (see section 4.5).
If the co-administration of REYATAZ with an NNRTI is required, an increase in the dose of both
REYATAZ and ritonavir to 400 mg and 200 mg, respectively, in combination with efavirenz could be
considered with close clinical monitoring.
Atazanavir is metabolised principally by CYP3A4. Co-administration of REYATAZ with ritonavir
and medicinal products that induce CYP3A4 is not recommended (see sections 4.3 and 4.5).
PDE5 inhibitors used for the treatment of erectile dysfunction: particular caution should be used when
prescribing PDE5-inhibitors (sildenafil, tadalafil, or vardenafil) for the treatment of erectile
dysfunction in patients receiving REYATAZ with concomitant low-dose ritonavir. Co-administration
of REYATAZ with these medicinal products is expected to substantially increase their concentrations
and may result in PDE5-associated adverse events such as hypotension, visual changes and priapism
(see section 4.5).
Co-administration of voriconazole and REYATAZ with ritonavir is not recommended unless an
assessment of the benefit/risk justifies the use of voriconazole (see section 4.5).
Concomitant use of REYATAZ/ritonavir and fluticasone or other glucocorticoids that are metabolized
by CYP3A4 is not recommended unless the potential benefit of treatment outweighs the risk of
systemic corticosteroid effects, including Cushing's syndrome and adrenal suppression
(see section 4.5).
Concomitant use of salmeterol and REYATAZ/ritonavir may result in increased cardiovascular
adverse events associated with salmeterol. Co-administration of salmeterol and REYATAZ is not
recommended (see section 4.5).
The absorption of atazanavir may be reduced in situations where gastric pH is increased irrespective of
cause.
Co-administration of REYATAZ with proton pump inhibitors is not recommended (see section 4.5). If
the combination of REYATAZ with a proton pump inhibitor is judged unavoidable, close clinical
monitoring is recommended in combination with an increase in the dose of REYATAZ to 400 mg with
100 mg of ritonavir; doses of proton pump inhibitors comparable to omeprazole 20 mg should not be
exceeded.
Co-administration of REYATAZ/ritonavir in combination with tenofovir and an H
2
-receptor
antagonist should be avoided (see section 4.5).
Lactose
Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or
glucose-galactose malabsorption should not take this medicinal product.
Paediatric population
Safety:
Asymptomatic PR interval prolongation was more frequent in paediatric patients than adults.
Asymptomatic first- and second-degree AV block was reported in paediatric patients (see section 4.8).
Caution should be used with medicinal products known to induce PR prolongations. In paediatric
patients with pre-existing conduction problems (second degree or higher atrioventricular or complex
bundle-branch block), REYATAZ should be used with caution and only if the benefits exceed the risk.
Cardiac monitoring is recommended based on the presence of clinical findings (e.g., bradycardia).
Efficacy
Atazanavir/ritonavir is not effective in viral strains harbouring multiple mutations of resistance. While
in adults no benefit can be expected in patients with
4 PI mutations, in treatment experienced
children even lower numbers of PI mutations may be predictive of a lack of benefit (see section 5.1).
4.5 Interaction with other medicinal products and other forms of interaction
When REYATAZ and ritonavir are co-administered, the metabolic drug interaction profile for
ritonavir may predominate because ritonavir is a more potent CYP3A4 inhibitor than atazanavir. The
Summary of Product Characteristics for ritonavir must be consulted before initiation of therapy with
REYATAZ and ritonavir.
Atazanavir is metabolised in the liver through CYP3A4. It inhibits CYP3A4. Therefore, REYATAZ
with ritonavir is contraindicated with medicinal products that are substrates of CYP3A4 and have a
narrow therapeutic index: astemizole, terfenadine, cisapride, pimozide, quinidine, bepridil, triazolam,
orally administered midazolam, and ergot alkaloids, particularly ergotamine and dihydroergotamine
(see section 4.3).
Other interactions
Interactions between atazanavir/ritonavir and protease inhibitors, antiretroviral agents other than
protease inhibitors, and other non-antiretroviral medicinal products are listed in the tables below
(increase is indicated as “↑”, decrease as “↓”, no change as “↔”, twice daily as “BID” and once daily
as “QD”). If available, 90% confidence intervals (CI) are shown in parentheses. The studies presented
in Table 2 were conducted in healthy subjects unless otherwise noted. Of importance, many studies
were conducted with unboosted atazanavir, which is not the approved regimen of atazanavir.
Table 2: Interactions between REYATAZ and other medicinal products
Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
ANTI-INFECTIVES
Antiretrovirals
Protease inhibitors:
The co-administration of REYATAZ/ritonavir and other protease inhibitors has not been studied but would be
expected to increase exposure to other protease inhibitors. Therefore, such co-administration is not recommended.
Ritonavir 100 mg QD
(atazanavir 300 mg QD)
studies conducted in HIV-
infected patients
Ritonavir 100 mg once
daily is used as a
booster of atazanavir
pharmacokinetics.
* In a combined analysis, atazanavir 300 mg and ritonavir 100 mg
(n=33) was compared to atazanavir 400 mg without ritonavir (n=28).
The mechanism of interaction between atazanavir and ritonavir is
CYP3A4 inhibition.
Indinavir is associated with indirect unconjugated hyperbilirubinaemia
due to inhibition of UGT.
Co-administration of
REYATAZ/ritonavir
and indinavir is not
recommended (see
section 4.4).
Nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs)
Lamivudine 150 mg BID +
zidovudine 300 mg BID
(atazanavir 400 mg QD)
No significant effect on lamivudine and zidovudine concentrations was
observed.
Based on these data
and because ritonavir
is not expected to have
a significant impact on
the pharmacokinetics
of NRTIs, the
co-administration of
REYATAZ/ritonavir
with these medicinal
products is not
expected to
significantly alter the
exposure of the co-
administered drugs.
The co-administration of REYATAZ/ ritonavir with abacavir is not
expected to significantly alter the exposure of abacavir.
Didanosine (buffered tablets)
200 mg/stavudine 40 mg, both
single dose (atazanavir 400 mg
Didanosine should be
taken at the fasted state
2 hours after











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
atazanavir,
simultaneous
administration
with ddI+d4T
(fasted)
REYATAZ/ritonavir
taken with food. The
co-administration of
REYATAZ/ritonavir
with stavudine is not
expected to
significantly alter the
exposure of stavudine.
atazanavir, dosed 1
hr after ddI+d4T
(fasted)
Atazanavir concentrations were greatly decreased when co-administered
with didanosine (buffered tablets) and stavudine. The mechanism of
interaction is a reduced solubility of atazanavir with increasing pH related
to the presence of anti-acid agent in didanosine buffered tablets.
No significant effect on didanosine and stavudine concentrations was
observed.
Didanosine (enteric coated
capsules) 400 mg single dose
(atazanavir 300 mg QD with
ritonavir 100 mg QD)
↑1.25
(0.92, 1.69)
No significant effect on atazanavir concentrations was observed when
administered with enteric-coated didanosine, but administration with food
decreased didanosine concentrations.
Tenofovir disoproxil fumarate
300 mg QD (atazanavir 300
mg QD with ritonavir 100 mg
QD) studies conducted in HIV-
infected patients
* In a combined analysis from several clinical studies,
atazanavir/ritonavir 300/100 mg co-administered with tenofovir
disoproxil fumarate 300 mg (n=39) was compared to
atazanavir/ritonavir 300/100 mg (n=33).
The efficacy of REYATAZ/ritonavir in combination with tenofovir in
treatment-experienced patients has been demonstrated in clinical study
045 and in treatment naive patients in clinical study 138 (see sections
4.8 and 5.1). The mechanism of interaction between atazanavir and
tenofovir is unknown.
Tenofovir disoproxil fumarate
300 mg QD (atazanavir 300
mg QD with ritonavir 100 mg
QD)
tenofovir
disoproxil
fumarate
Patients should be
closely monitored for
tenofovir-associated
adverse events,
including renal
disorders.
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Efavirenz 600 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (pm):
all administered
with food
Co-administration of
efavirenz with
REYATAZ/ritonavir is
not recommended (see
section 4.4)
Efavirenz 600 mg QD
(atazanavir 400 mg QD with
ritonavir 200 mg QD)
↔1.12*/**
(0.84, 1.49)
* When compared to REYATAZ 300 mg/ritonavir 100 mg once daily in
the evening without efavirenz. This decrease in atazanavir C
min
, might
negatively impact the efficacy of atazanavir. The mechanism of
efavirenz/atazanavir interaction is CYP3A4 induction.
** based on historical comparison.
Nevirapine 200 mg BID
(atazanavir 400 mg QD with
ritonavir 100 mg QD) study
conducted in HIV infected
patients
Co-administration of
nevirapine with
REYATAZ/ritonavir is
not recommended (see
section 4.4)
↓0.41*
(0.27, 0.60)
* When compared to REYATAZ 300 mg and ritonavir 100 mg without
nevirapine. This decrease in atazanavir C
min
, might negatively impact
the efficacy of atazanavir. The mechanism of nevirapine/atazanavir
interaction is CYP3A4 induction.
Integrase Inhibitors
Raltegravir 400 mg BID
(atazanavir/ritonavir)
No dose adjustment
required for Isentress.
The mechanism is UGT1A1 inhibition.
atazanavir (pm):
all administered
with food











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
Antibiotics
Clarithromycin 500 mg BID
(atazanavir 400 mg QD)
No recommendation
regarding dose
reduction can be made;
therefore, caution
should be exercised if
REYATAZ/ritonavir is
co-administered with
clarithromycin.
A dose reduction of clarithromycin may result in subtherapeutic
concentrations of 14-OH clarithromycin. The mechanism of the
clarithromycin/atazanavir interaction is CYP3A4 inhibition.
Antifungals
Ketoconazole 200 mg QD
(atazanavir 400 mg QD)
No significant effect on atazanavir concentrations was observed.
Ketoconazole and
itraconazole should be
used cautiously with
REYATAZ/ritonavir.
High doses of
ketoconazole and
itraconazole (>200
mg/day) are not
recommended.
Itraconazole, like ketoconazole, is a potent inhibitor as well as a
substrate of CYP3A4.
Based on data obtained with other boosted PIs and ketoconazole, where
ketoconazole AUC showed a 3-fold increase, REYATAZ/ritonavir is
expected to increase ketoconazole or itraconazole concentrations.
Co-administration of REYATAZ/ritonavir and voriconazole has not
been studied.
Co-administration of
voriconazole and
REYATAZ/ritonavir is
not recommended
unless an assessment
of the benefit/risk to
the patient justifies the
use of voriconazole
(see section 4.4).
Patients should be
carefully monitored for
adverse events and/or
loss of efficacy during
the co-administration
of voriconazole and
REYATAZ/ritonavir.
The effect of co-administration of oral voriconazole and low dose (100
mg) oral ritonavir was investigated in healthy volunteers. Low doses of
ritonavir (100 mg BID) decreased the C
max
and AUC of voriconazole
(90% CI) by an average of 24% (↓9% to ↓36%) and 39% (↓22% to
↓52%), respectively. Administration of voriconazole resulted in a minor
decrease in steady state C
max
and AUC of ritonavir (90% CI) with an
average of 24% (↓6% to ↓39%) and 14% (↓26% to ↑1%), respectively.
Fluconazole 200 mg QD
(atazanavir 300 mg and
ritonavir 100 mg QD)
Atazanavir and fluconazole concentrations were not significantly
modified when REYATAZ/ritonavir was co-administered with
fluconazole.
No dosage adjustments
are needed for
REYATAZ/ritonavir
and fluconazole.
Antimycobacterial
Rifabutin 150 mg twice weekly
(atazanavir 300 mg and
ritonavir 100 mg QD)
When given with
REYATAZ/ritonavir,
the recommended dose
of rifabutin is 150 mg
3 times per week on set
days (for example
Monday-Wednesday-
Friday). Increased
monitoring for
rifabutin-associated
adverse reactions
including neutropenia
and uveitis is
warranted due to an
expected increase in
exposure to rifabutin.
Further dosage
reduction of rifabutin
to 150 mg twice
weekly on set days is
recommended for
25-O-desacetyl-
rifabutin
** When compared to rifabutin 150 mg QD alone. Total rifabutin and
25-O-desacetyl-rifabutin AUC: ↑2.19 (1.78, 2.69).
In previous studies, the pharmacokinetics of atazanavir was not altered
by rifabutin.











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
patients in whom the
150 mg dose 3 times
per week is not
tolerated. It should be
kept in mind that the
twice weekly dosage of
150 mg may not
provide an optimal
exposure to rifabutin
thus leading to a risk of
rifamycin resistance
and a treatment failure.
No dose adjustment is
needed for
REYATAZ/ritonavir.
Rifampicin is a strong CYP3A4 inducer and has been shown to cause a 72%
decrease in atazanavir AUC which can result in virological failure and
resistance development. During attempts to overcome the decreased exposure
by increasing the dose of REYATAZ or other protease inhibitors with
ritonavir, a high frequency of liver reactions was seen.
The combination of
rifampicin and
REYATAZ with
concomitant low-dose
ritonavir is
contraindicated
(see section 4.3).
ACID REDUCING AGENTS
H
2
-Receptor antagonists
For patients not
taking tenofovir,
if
REYATAZ 300
mg/ritonavir 100 mg
and H
2
-receptor
antagonists are
co-administered, a
dose equivalent to
famotidine 20 mg BID
should not be
exceeded. If a higher
dose of an H
2
-receptor
antagonist is required
(eg, famotidine 40 mg
BID or equivalent) an
increase of the
REYATAZ/ritonavir
dose from 300/100 mg
to 400/100 mg can be
considered.
In HIV-infected patients with atazanavir/ritonavir at
the recommended dose 300/100 mg QD
In Healthy volunteers with atazanavir/ritonavir at an
increased dose of 400/100 mg QD
atazanavir ↔1.03
(0.86, 1.22)
In HIV-infected patients with atazanavir/ritonavir at
the recommended dose of 300/100 mg QD
For patients who are
taking tenofovir,
Co-administration of
REYATAZ/ritonavir in
combination with
tenofovir and an
H
2
-receptor antagonist
should be avoided
(see section 4.4). If the
combination of
REYATAZ/ritonavir
with both tenofovir and
an H
2
-receptor
antagonist is judged
unavoidable, close
clinical monitoring is
recommended. A dose
increase of REYATAZ
to 400 mg with 100 mg
of ritonavir may be
atazanavir ↓0.79*
(0.66, 0.96)
atazanavir ↓0.76*
(0.64, 0.89)
* When compared to atazanavir 300 mg QD with ritonavir 100 mg QD
and tenofovir disoproxil fumarate 300 mg all as a single dose with food.
When compared to atazanavir 300 mg with ritonavir 100 mg
without
tenofovir
, atazanavir concentrations are expected to be additionally
decreased by about 20%.
The mechanism of interaction is decreased solubility of atazanavir as
intra-gastric pH increases with H
2
blockers.















Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
considered but is still
under evaluation.
Omeprazole 40 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (am): 2
hr after
omeprazole
Co-administration of
REYATAZ/ritonavir
with proton pump
inhibitors is not
recommended. If the
combination of
REYATAZ/ritonavir
with a proton pump
inhibitor is judged
unavoidable, close
clinical monitoring is
recommended in
combination with an
increase in the dose of
REYATAZ to 400 mg
with 100 mg of
ritonavir; doses of
proton pump inhibitors
comparable to
omeprazole 20 mg
should not be exceeded
(see section 4.4).
Omeprazole 20 mg QD
(atazanavir 400 mg QD with
ritonavir 100 mg QD)
atazanavir (am): 1
hr after
omeprazole
* When compared to atazanavir 300 mg QD with ritonavir 100 mg QD
The decrease in AUC, C
max
, and C
min
was not mitigated when an
increased dose of REYATAZ/ritonavir (400/100 mg once daily) was
temporally separated from omeprazole by 12 hours. Although not
studied, similar results are expected with other proton pump inhibitors.
This decrease in atazanavir exposure might negatively impact the
efficacy of atazanavir. The mechanism of interaction is decreased
solubility of atazanavir as intra-gastric pH increases with proton pump
inhibitors.
Antacids and medicinal
products containing buffers
Reduced plasma concentrations of atazanavir may be the consequence of
increased gastric pH if antacids, including buffered medicinal products,
are administered with REYATAZ/ritonavir.
REYATAZ/ritonavir
should be administered
2 hours before or 1
hour after antacids or
buffered medicinal
products.
ALPHA 1-ADRENORECEPTOR ANTAGONIST
Alfuzosin
Potential for increased alfuzosin concentrations which can result in
hypotension. The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Co-administration of
REYATAZ/ritonavir
with alfuzosin is
contraindicated (see
section 4.3)
Co-administration with REYATAZ/ritonavir has the potential to
produce a decrease or, less often, an increase in INR (International
Normalised Ratio).
It is recommended that
the INR be monitored
carefully during
treatment with
REYATAZ/ritonavir,
especially when
commencing therapy.
ANTINEOPLASTICS AND IMMUNOSUPRESSANTS
Atazanavir inhibits UGT and may interfere with the metabolism of
irinotecan, resulting in increased irinotecan toxicities.
If REYATAZ/ritonavir
is co-administered with
irinotecan, patients
should be closely
monitored for adverse
events related to
irinotecan.
Cyclosporin
Tacrolimus
Sirolimus
Concentrations of these immunosuppressants may be increased when
co-administered with REYATAZ/ritonavir due to CYP3A4 inhibition.
More frequent
therapeutic
concentration
monitoring of these
medicinal products is
recommended until
plasma levels have
been stabilised.














Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
Amiodarone,
Systemic lidocaine,
Quinidine
Concentrations of these antiarrhythmics may be increased when
co-administered with REYATAZ/ritonavir. The mechanism of
amiodarone or systemic lidocaine/atazanavir interaction is CYP3A
inhibition. Quinidine has a narrow therapeutic window and is
contraindicated due to potential inhibition of CYP3A by
REYATAZ/ritonavir.
Caution is warranted
and therapeutic
concentration
monitoring is
recommended when
available. The
concomitant use of
quinidine is
contraindicated
(see section 4.3).
REYATAZ/ritonavir should not be used in combination with medicinal
products that are substrates of CYP3A4 and have a narrow therapeutic
index.
Co-administration with
bepridil is
contraindicated (see
section 4.3)
Diltiazem 180 mg QD
(atazanavir 400 mg QD)
An initial dose
reduction of diltiazem
by 50% is
recommended, with
subsequent titration as
needed and ECG
monitoring.
No significant effect on atazanavir concentrations was observed. There
was an increase in the maximum PR interval compared to atazanavir
alone. Co-administration of diltiazem and REYATAZ/ritonavir has not
been studied. The mechanism of diltiazem/atazanavir interaction is
CYP3A4 inhibition.
Serum concentrations of verapamil may be increased by
REYATAZ/ritonavir due to CYP3A4 inhibition.
Caution should be
exercised when
verapamil is
co-administered with
REYATAZ/ritonavir.
Fluticasone propionate
intranasal 50 µg 4 times daily
for 7 days (ritonavir 100 mg
capsules BID)
The fluticasone propionate plasma levels increased significantly,
whereas the intrinsic cortisol levels decreased by approximately 86%
(90% confidence interval 82-89%) Greater effects may be expected
when fluticasone propionate is inhaled. Systemic corticosteroid effects
including Cushing’s syndrome and adrenal suppression have been
reported in patients receiving ritonavir and inhaled or intranasally
administered fluticasone propionate; this could also occur with other
corticosteroids metabolized via the P450 3A pathway, e.g., budesonide.
The effects of high fluticasone systemic exposure on ritonavir plasma
levels are yet unknown. The mechanism of interaction is CYP3A4
inhibition.
Co-administration of
REYATAZ/ritonavir
and these
glucocorticoids is not
recommended unless
the potential benefit of
treatment outweighs
the risk of systemic
corticosteroid effects
(see section 4.4). A
dose reduction of the
glucocorticoid should
be considered with
close monitoring of
local and systemic
effects or a switch to a
glucocorticoid, which
is not a substrate for
CYP3A4 (e.g.,
beclomethasone).
Moreover, in case of
withdrawal of
glucocorticoids,
progressive dose
reduction may have to
be performed over a
longer period.
Sildenafil, tadalafil, vardenafil Sildenafil, tadalafil, and vardenafil are metabolised by CYP3A4.
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of the PDE5 inhibitor and an increase in
PDE5-associated adverse events, including hypotension, visual changes,
Patients should be
warned about these
possible side effects
when using PDE5











Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
and priapism. The mechanism of this interaction is CYP3A4 inhibition.
inhibitors for erectile
dysfunction with
REYATAZ/ritonavir
(see section 4.4).
Also see
PULMONARY
ATERIAL
HYPERTENSION in
this table for futher
information regarding
co-administration of
REYATAZ/ritonavir
with sildenafil.
St. John’s wort (Hypericum
perforatum):
Concomitant use of St. John's wort with REYATAZ/ritonavir may be
expected to result in significant reduction in plasma levels of atazanavir.
This effect may be due to an induction of CYP3A4. There is a risk of
loss of therapeutic effect and development of resistance (see section
4.3).
Co-administration of
REYATAZ/ritonavir
with products
containing St. John's
wort is contraindicated.
Ethinyloestradiol 25 μg +
norgestimate (atazanavir 300
mg QD with ritonavir 100 mg
QD)
If an oral contraceptive
is administered with
REYATAZ/ritonavir, it
is recommended that
the oral contraceptive
contain at least 30 μg
of ethinyloestradiol
and that the patient be
reminded of strict
compliance with this
contraceptive dosing
regimen. Co-
administration of
REYATAZ/ritonavir
with other hormonal
contraceptives or oral
contraceptives
containing
progestogens other
than norgestimate has
not been studied, and
therefore should be
avoided. An alternate
reliable method of
contraception is
recommended.
↑2.02
(1.77, 2.31)
While the concentration of ethinyloestradiol was increased with
atazanavir given alone, due to both UGT and CYP3A4 inhibition by
atazanavir, the net effect of atazanavir/ritonavir is a decrease in
ethinyloestradiol levels because of the inducing effect of ritonavir.
The increase in progestin exposure may lead to related side-effects (e.g.
insulin resistance, dyslipidemia, acne and spotting), thus possibly
affecting the compliance.
LIPID LOWERING AGENTS
HMG-CoA reductase inhibitors
Simvastatin
Lovastatin
Simvastatin and lovastatin are highly dependent on CYP3A4 for their
metabolism and co-administration with REYATAZ/ritonavir may result
in increased concentrations.
Co-administration of
simvastatin or
lovastatin with
REYATAZ/ritonavir is
not recommended due
to an increased risk of
myopathy including
rhabdomyolysis. The
use of another HMG-
CoA reductase
inhibitor which does
not undergo
metabolism by CYP3A
such as pravastatin or
fluvastatin is








Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
The risk of myopathy including rhabdomyolysis may also be increased
with atorvastatin, which is also metabolised by CYP3A4.
Caution should be
exercised.
INHALED BETA AGONISTS
Salmeterol
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of salmeterol and an increase in salmeterol-associated
adverse events.
Co-administration of
salmeterol with
REYATAZ/ritonavir is
not recommended (see
section 4.4).
The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Buprenorphine, QD, stable
maintenance dose,
(atazanavir 300 mg QD with
ritonavir 100 mg QD)
Co-administration
warrants
clinical monitoring for
sedation and cognitive
effects. A dose
reduction of
buprenorphine may be
considered
norbuprenorphine ↑2.05 ↑1.61 ↑2.01
The mechanism of interaction is CYP3A4 and UGT1A1 inhibition.
Concentrations of atazanavir were not significantly affected.
Methadone, stable maintenance
dose
(atazanavir 400 mg QD)
No significant effect on methadone concentrations was observed. Given
that low dose ritonavir (100 mg twice daily) has been shown to have no
significant effect on methadone concentrations, no interaction is
expected if methadone is co-administered with REYATAZ and
ritonavir, based on these data.
No dosage adjustment
is necessary if
methadone is
co-administered with
REYATAZ and
ritonavir.
PULMONARY ARTERIAL HYPERTENSION
PDE5 Inhibitors
Co-administration with REYATAZ/ritonavir may result in increased
concentrations of the PDE5 inhibitor and an increase in PDE5-inhibitor-
associated adverse events.
A safe and effective
dose in combination
with
REYATAZ/ritonavir
has not been
established for
sildenafil when used to
treat pulmonary arterial
hypertension.
Sildenafil, when used
for the treatment of
pulmonary arterial
hypertension, is
contraindicated (see
section 4.3).
The mechanism of interaction is CYP3A4 inhibition by
atazanavir/ritonavir.
Midazolam and triazolam are extensively metabolized by CYP3A4.
Co-administration with REYATAZ/ritonavir may cause a large increase
in the concentration of these benzodiazepines. No drug interaction study
has been performed for the co-administration of REYATAZ/ritonavir
with benzodiazepines. Based on data for other CYP3A4 inhibitors,
plasma concentrations of midazolam are expected to be significantly
higher when midazolam is given orally. Data from concomitant use of
parenteral midazolam with other protease inhibitors suggest a possible
3-4 fold increase in midazolam plasma levels.
REYATAZ/ritonavir
should not be
co-administered with
triazolam or orally
administered
midazolam (see section
4.3), whereas caution
should be used with
co-administration of
REYATAZ/ritonavir
and parenteral
midazolam. If
REYATAZ is
co-administered with
parenteral midazolam,
it should be done in an
intensive care unit
(ICU) or similar setting
which ensures close
clinical monitoring and
appropriate medical













Co-administered medicinal
products (dose in mg)
Medicinal
product assessed
Recommendations
concerning
co-administration
management in case of
respiratory depression
and/or prolonged
sedation. Dosage
adjustment for
midazolam should be
considered, especially
if more than a single
dose of midazolam is
administered.
4.6 Pregnancy and lactation
There are no adequate data from the use of atazanavir in pregnant women. Studies in animals have not
shown evidence of selective developmental toxicity or effects on reproductive function and fertility
(see section 5.3). REYATAZ should be used during pregnancy only if the potential benefit justifies the
potential risk.
It is not known whether REYATAZ administered to the mother during pregnancy will exacerbate
physiological hyperbilirubinaemia and lead to kernicterus in neonates and infants. In the prepartum
period, additional monitoring and alternative therapy to REYATAZ should be considered.
It is not known whether atazanavir is excreted in human milk. Studies in rats have demonstrated that
atazanavir is excreted in the milk. It is therefore recommended that mothers being treated with
REYATAZ not breast-feed their infants. As a general rule, it is recommended that HIV infected
women not breast-feed their infants in order to avoid transmission of HIV.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. Patients
should be informed that dizziness has been reported during treatment with regimens containing
REYATAZ (see section 4.8).
REYATAZ has been evaluated for safety in combination therapy with other antiretroviral medicinal
products in controlled clinical trials in 1,806 adult patients receiving REYATAZ 400 mg once daily
(1,151 patients, 52 weeks median duration and 152 weeks maximum duration) or REYATAZ 300 mg
with ritonavir 100 mg once daily (655 patients, 96°weeks median duration and 108 weeks maximum
duration).
Adverse reactions were consistent between patients who received REYATAZ 400 mg once daily and
patients who received REYATAZ 300 mg with ritonavir 100 mg once daily, except that jaundice and
elevated total bilirubin levels were reported more frequently with REYATAZ plus ritonavir.
Among patients who received REYATAZ 400 mg once daily or REYATAZ 300 mg with ritonavir
100 mg once daily, the only adverse reactions of any severity reported very commonly with at least a
possible relationship to
regimens containing REYATAZ and one or more NRTIs were nausea (20%),
diarrhoea (10%), and jaundice (13%). Among patients receiving REYATAZ 300 mg with ritonavir
100 mg, the frequency of jaundice was 19%. In the majority of cases, jaundice was reported within a
few days to a few months after the initiation of treatment (see section 4.4).
Combination antiretroviral therapy has been associated with redistribution of body fat (lipodystrophy)
in HIV patients, including loss of peripheral and facial subcutaneous fat, increased intra-abdominal
and visceral fat, breast hypertrophy, and dorsocervical fat accumulation (buffalo hump).


Combination antiretroviral therapy has been associated with metabolic abnormalities such as
hypertriglyceridaemia, hypercholesterolaemia, insulin resistance, hyperglycaemia, and
hyperlactataemia (see sections 4.4 and 5.1).
Adult patients
The following adverse reactions of moderate intensity or greater with at least a possible relationship to
regimens containing REYATAZ and one or more NRTIs have also been reported. The frequency of
adverse reactions listed below is defined using the following convention: very common (≥ 1/10),
common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), or
very rare (< 1/10,000). Within each frequency grouping, undesirable effects are presented in order of
decreasing seriousness.
rare: oedema, palpitation
Nervous system disorders:
common: headache;
uncommon: peripheral neuropathy, syncope, amnesia,
dizziness, somnolence, dysgeusia
Respiratory, thoracic and
mediastinal disorders:
Gastrointestinal disorders:
common: vomiting, diarrhoea, abdominal pain, nausea,
dyspepsia;
uncommon: pancreatitis, gastritis, abdominal distension,
stomatitis aphthous, flatulence, dry mouth
Renal and urinary disorders:
uncommon: nephrolithiasis, hematuria, proteinuria,
pollakiuria;
rare: kidney pain
Skin and subcutaneous tissue
disorders:
common: rash;
uncommon: urticaria, alopecia, pruritus;
rare: vesiculobullous rash, eczema, vasodilatation
Musculoskeletal and connective
tissue disorders:
uncommon: muscle atrophy, arthralgia, myalgia;
rare: myopathy
Metabolism and nutrition
disorders:
uncommon: weight decreased, weight gain, anorexia,
appetite increased
General disorders and
administration site conditions:
common: lipodystrophy syndrome, fatigue;
uncommon: chest pain, malaise, pyrexia, asthenia;
rare: gait disturbance
uncommon: hypersensitivity
common: jaundice;
uncommon: hepatitis;
rare: hepatosplenomegaly
Reproductive system and breast
disorders:
uncommon: depression, disorientation, anxiety, insomnia,
sleep disorder, abnormal dream
In HIV-infected patients with severe immune deficiency at the time of initiation of combination
antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic
infections may arise (see section 4.4).
Cases of osteonecrosis have been reported, particularly in patients with generally acknowledged risk
factors, advanced HIV disease or long-term exposure to combination antiretroviral therapy (CART).
The frequency of this is unknown (see section 4.4).
Laboratory abnormalities
The most frequently reported laboratory abnormality in patients receiving regimens containing
REYATAZ and one or more NRTIs was elevated total bilirubin reported predominantly as elevated
indirect [unconjugated] bilirubin (87% Grade 1, 2, 3, or 4). Grade 3 or 4 elevation of total bilirubin
was noted in 37% (6% Grade 4). Among experienced patients treated with REYATAZ 300 mg once
daily with 100 mg ritonavir once daily for a median duration of 95 weeks, 53% had Grade 3-4 total
bilirubin elevations. Among naive patients treated with REYATAZ 300 mg once daily with 100 mg
ritonavir once daily for a median duration of 96 weeks, 48% had Grade 3-4 total bilirubin elevations
(see section 4.4).
Other marked clinical laboratory abnormalities (Grade 3 or 4) reported in ≥ 2% of patients receiving
regimens containing REYATAZ and one or more NRTIs included: elevated creatine kinase (7%),
elevated alanine aminotransferase/serum glutamic-pyruvic transaminase (ALT/SGPT) (5%), low
neutrophils (5%), elevated aspartate aminotransferase/serum glutamic-oxaloacetic transaminase
(AST/SGOT) (3%), and elevated lipase (3%).
Two percent of patients treated with REYATAZ experienced concurrent Grade 3-4 ALT/AST and
Grade 3-4 total bilirubin elevations.
Patients co-infected with hepatitis B and/or hepatitis C virus
Among 1,151 patients receiving atazanavir 400 mg once daily, 177 patients were co-infected with
chronic hepatitis B or C, and among 655 patients receiving atazanavir 300 mg once daily with
ritonavir 100 mg once daily, 97 patients were co-infected with chronic hepatitis B or C. Co-infected
patients were more likely to have baseline hepatic transaminase elevations than those without chronic
viral hepatitis. No differences in frequency of bilirubin elevations were observed between these
patients and those without viral hepatitis. The frequency of treatment emergent hepatitis or
transaminase elevations in co-infected patients was comparable between REYATAZ and comparator
regimens (see section 4.4).
Paediatric population
In clinical studies, paediatric patients 3 months to less than 18 years of age had a mean duration of
treatment with REYATAZ of 115 weeks. The safety profile in these studies was overall comparable to
that seen in adults. Both asymptomatic first-degree (23%) and second-degree (1%) atrioventricular
block were reported in paediatric patients. The most frequently reported laboratory abnormality in
paediatric patients receiving REYATAZ was elevation of total bilirubin (≥ 2.6 times ULN , Grade 3-4)
which occurred in 45% of patients.
Postmarketing experience
There have been postmarketing reports of unknown frequency for torsades de pointes, QTc
prolongation, diabetes mellitus, hyperglycaemia, nephrolithiasis, and gallbladder disorders including
cholelithiasis, cholecystitis, and cholestasis.
Human experience of acute overdose with REYATAZ is limited. Single doses up to 1,200 mg have
been taken by healthy volunteers without symptomatic untoward effects. At high doses that lead to
high drug exposures, jaundice due to indirect (unconjugated) hyperbilirubinaemia (without associated
liver function test changes) or PR interval prolongations may be observed (see sections 4.4 and 4.8).
Treatment of overdose with REYATAZ should consist of general supportive measures, including
monitoring of vital signs and electrocardiogram (ECG), and observations of the patient's clinical
status. If indicated, elimination of unabsorbed atazanavir should be achieved by emesis or gastric
lavage. Administration of activated charcoal may also be used to aid removal of unabsorbed drug.
There is no specific antidote for overdose with REYATAZ. Since atazanavir is extensively
metabolised by the liver and is highly protein bound, dialysis is unlikely to be beneficial in significant
removal of this medicinal product.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group: protease inhibitor, ATC code: J05AE08
Mechanism of action:
atazanavir is an azapeptide HIV-1 protease inhibitor (PI). The compound
selectively inhibits the virus-specific processing of viral Gag-Pol proteins in HIV-1 infected cells, thus
preventing formation of mature virions and infection of other cells.
Antiviral activity
in vitro:
atazanavir exhibits anti-HIV-1 (including all clades tested) and anti-HIV-2
activity in cell culture.
Resistance
Antiretroviral treatment naive adult patients
In clinical trials of antiretroviral treatment naive patients treated with unboosted atazanavir, the I50L
substitution, sometimes in combination with an A71V change, is the signature resistance substitution
for atazanavir. Resistance levels to atazanavir ranged from 3.5- to 29-fold without evidence of
phenotypic cross resistance to other PIs. In clinical trials of antiretroviral treatment naive patients
treated with boosted atazanavir, the I50L substitution did not emerge in any patient without baseline PI
substitutions. The N88S substitution has been rarely observed in patients with virologic failure on
atazanavir (with or without ritonavir). While it may contribute to decreased susceptibility to atazanavir
when it occurs with other protease substitutions, in clinical studies N88S by itself does not always lead
to phenotypic resistance to atazanavir or have a consistent impact on clinical efficacy.
Table 3. De novo substitutions in treatment naive patients failing therapy with atazanavir +
ritonavir (Study 138, 96 weeks)
Frequency de novo PI substitution (n=26)
a
>20% none
10-20% none
a
Number of patients with paired genotypes classified as virological failures (HIV RNA ≥ 400 copies/ml).
The M184I/V substitution emerged in 5/26 REYATAZ/ritonavir and 7/26 lopinavir/ritonavir virologic
failure patients, respectively.
Antiretroviral treatment experienced adult patients
In antiretroviral treatment experienced patients from Studies 009, 043, and 045, 100 isolates from
patients designated as virological failures on therapy that included either atazanavir, atazanavir +
ritonavir, or atazanavir + saquinavir were determined to have developed resistance to atazanavir. Of
the 60 isolates from patients treated with either atazanavir or atazanavir + ritonavir, 18 (30%)
displayed the I50L phenotype previously described in naive patients.
Table 4. De novo substitutions in treatment experienced patients failing therapy with atazanavir
+ ritonavir (Study 045, 48 weeks)
Frequency
de novo PI substitution (n=35)
a,b




>20% M36, M46, I54, A71, V82
10-20% L10, I15, K20, V32, E35, S37, F53, I62, G73, I84, L90
a
Number of patients with paired genotypes classified as virological failures (HIV RNA ≥ 400 copies/ml).
b
Ten patients had baseline phenotypic resistance to atazanavir + ritonavir (fold change [FC]>5.2). FC susceptibility in cell
culture relative to the wild-type reference was assayed using PhenoSense
TM
(Monogram Biosciences, South San Francisco,
California, USA)
None of the de novo substitutions (see Table 4) are specific to atazanavir and may reflect re-
emergence of archived resistance on atazanavir + ritonavir in Study 045 treatment-experienced
population.
The resistance in antiretroviral treatment experienced patients mainly occurs by accumulation of the
major and minor resistance substitutions described previously to be involved in protease inhibitor
resistance.
Clinical results
In antiretroviral naive adult patients
Study 138
is an international randomised, open-label, multicenter, prospective trial of treatment naïve
patients comparing REYATAZ/ritonavir (300 mg/100 mg once daily) to lopinavir/ritonavir
(400 mg/100 mg twice daily), each in combination with fixed dose tenofovir/emtricitabine
(300 mg/200 mg tablets once daily). The REYATAZ/ritonavir arm showed similar (non-inferior)
antiviral efficacy compared to the lopinavir/ritonavir arm, as assessed by the proportion of patients
with HIV RNA < 50 copies/ml at week 48 (Table 5).
Analyses of data through 96 weeks of treatment demonstrated durability of antiviral activity (Table 5).

Table 5: Efficacy Outcomes in Study 138
a
REYATAZ/ritonavir
b
(300 mg/100 mg once daily)
n=440
Lopinavir/ritonavir
c
(400 mg/100 mg twice daily)
n=443
HIV RNA <50 copies/ml, %
All patients
d
Difference estimate
[95% CI]
d
Week 48: 1.7% [-3.8%, 7.1%]
Week 96: 6.1% [0.3%, 12.0%]
Week 48: -3% [-7.6%, 1.5%]
Week 96: 2.2% [-2.3%, 6.7%]
HIV RNA <50 copies/ml, % by Baseline Characteristic
d
HIV RNA
<100,000 copies/ml
HIV RNA Mean Change from Baseline, log
10
copies/ml
All patients
CD4 Mean Change from Baseline, cells/mm
3
All patients
CD4 Mean Change from Baseline, cells/mm
3
by Baseline Characteristic
HIV RNA
<100,000 copies/ml
≥100,000 copies/ml 227 (n=187) 291 (n=173) 245 (n=180) 310 (n=165)
a
Mean baseline CD4 cell count was 214 cells/mm
3
(range 2 to 810 cells/mm
3
) and mean baseline plasma HIV-1 RNA was
4.94 log
10
copies/ml (range 2.6 to 5.88 log
10
copies/ml)
b
REYATAZ/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
c
Lopinavir/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
d
Intent-to-treat analysis, with missing values considered as failures.
e
Per protocol analysis: Excluding non-completers and patients with major protocol deviations.
f
Number of patients evaluable.
In antiretroviral experienced adult patients
Study 045
is a randomised, multicenter trial comparing REYATAZ/ritonavir (300/100 mg once daily)
and REYATAZ/saquinavir (400/1,200 mg once daily), to lopinavir + ritonavir (400/100 mg fixed dose
combination twice daily), each in combination with tenofovir (see sections 4.5 and 4.8) and one NRTI,
in patients with virologic failure on two or more prior regimens containing at least one PI, NRTI, and
NNRTI. For randomised patients, the mean time of prior antiretroviral exposure was 138 weeks for
PIs, 281 weeks for NRTIs, and 85 weeks for NNRTIs. At baseline, 34% of patients were receiving a
PI and 60% were receiving an NNRTI. Fifteen of 120 (13%) patients in the REYATAZ + ritonavir
treatment arm and 17 of 123 (14%) patients in the lopinavir + ritonavir arm had four or more of the PI
substitutions L10, M46, I54, V82, I84, and L90. Thirty-two percent of patients in the study had a viral
strain with fewer than two NRTI substitutions.
The primary endpoint was the time-averaged difference in change from baseline in HIV RNA through
48 weeks (Table 6).
Difference estimate
e
[95% CI]
























Table 6: Efficacy Outcomes at Week 48
a
and at Week 96 (Study 045)
ATV/RTV
b
(300 mg/
100 mg once daily)
n=120
LPV/RTV
c
(400 mg/
100 mg twice daily)
n=123
Time-averaged difference
ATV/RTV-LPV/RTV
[97.5% CI
d
]
HIV RNA Mean Change from Baseline, log
10
copies/ml
All patients
HIV RNA <50 copies/ml, %
f
(responder/evaluable)
All patients
36 (43/120) 32 (38/120) 42 (52/123 35 (41/118)
HIV RNA <50 copies/ml by select baseline PI substitutions,
f, g
% (responder/evaluable)
0-2
CD4 Mean Change from Baseline, cells/mm
3
All patients 110 (n=83) 122 (n=60) 121 (n=94) 154 (n=60) NA NA
a
The mean baseline CD4 cell count was 337 cells/mm
3
(range: 14 to 1,543 cells/mm
3
) and the mean baseline plasma HIV-1
RNA level was 4.4 log
10
copies/ml (range: 2.6 to 5.88 log
10
copies/ml).
b
ATV/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
c
LPV/RTV with tenofovir/emtricitabine (fixed dose 300 mg/200 mg tablets once daily).
d
Confidence interval.
e
Number of patients evaluable.
f
Intent-to-treat analysis, with missing values considered as failures. Responders on LPV/RTV who completed treatment
before Week 96 are excluded from Week 96 analysis. The proportion of patients with HIV RNA < 400 copies/ml were 53%
and 43% for ATV/RTV and 54% and 46% for LPV/RTV at weeks 48 and 96 respectively.
g
Select substitutions include any change at positions L10, K20, L24, V32, L33, M36, M46, G48, I50, I54, L63, A71, G73,
V82, I84, and L90 (0-2, 3, 4 or more) at baseline.
NA = not applicable.
Through 48 weeks of treatment, the mean changes from baseline in HIV RNA levels for REYATAZ +
ritonavir and lopinavir + ritonavir were similar (non-inferior). Consistent results were obtained with
the last observation carried forward method of analysis (time-averaged difference of 0.11, 97.5%
confidence interval [-0.15, 0.36]). By as-treated analysis, excluding missing values, the proportions of
patients with HIV RNA < 400 copies/ml (< 50 copies/ml) in the REYATAZ + ritonavir arm and the
lopinavir + ritonavir arm were 55% (40%) and 56% (46%), respectively.
Through 96 weeks of treatment, mean HIV RNA changes from baseline for REYATAZ + ritonavir
and lopinavir + ritonavir met criteria for non-inferiority based on observed cases. Consistent results
were obtained with the last observation carried forward method of analysis. By as-treated analysis,
excluding missing values, the proportions of patients with HIV RNA <400 copies/ml (<50 copies/ml)
for REYATAZ + ritonavir were 84% (72%) and for lopinavir + ritonavir were 82% (72%). It is
important to note that at time of the 96-week analysis, 48 % of patients overall remained on study.
REYATAZ + saquinavir was shown to be inferior to lopinavir + ritonavir.
Paediatric population
Assessment of the pharmacokinetics, safety, tolerability, and efficacy of REYATAZ is based on data
from the open-label, multicenter clinical trial PACTG 1020A conducted in patients from 3 months to
21 years of age. Overall in this study, 182 paediatric patients (81 antiretroviral-naive and
101 antiretroviral-experienced) received once daily REYATAZ (capsule or powder formulation), with
or without ritonavir, in combination with two NRTIs.
The clinical data derived from this study are inadequate to support the use of atazanavir (with or
without ritonavir) in children below 6 years of age.
Efficacy data observed in the 41 paediatric patients aged 6 years to less than 18 years that received
REYATAZ capsules with ritonavir are presented in Table 7. For treatment-naive paediatric patients,
the mean baseline CD4 cell count was 344 cells/mm
3
(range: 2 to 800 cells/ mm
3
) and mean baseline



















plasma HIV 1 RNA was 4.67 log
10
copies/ml (range: 3.70 to 5.00 log
10
copies/ml). For treatment-
experienced paediatric patients, the mean baseline CD4 cell count was 522 cells/mm
3
(range: 100 to
1157 cells/ mm
3
) and mean baseline plasma HIV 1 RNA was 4.09 log
10
copies/ml (range: 3.28 to
5.00 log
10
copies/ml).
Table 7: Efficacy Outcomes (paediatric patients 6 years to less than 18 years of age) at Week
48 (Study PACTG 1020A)
Treatment-Naive
REYATAZ
Capsules/ritonavir
(300 mg/100 mg once
daily) n=16
Treatment-
Experienced
REYATAZ
Capsules/ritonavir
(300 mg/100 mg once
daily) n=25
HIV RNA <50 copies/ml, %
a
All patients
HIV RNA <400 copies/ml, %
a
All patients
CD4 Mean Change from Baseline, cells/mm
3
All patients 293 (n=14
b
)
229 (n=14
b
)
HIV RNA <50 copies/ml by select baseline PI substitutions,
c
% (
responder/evaluable
d
)
0-2
a
Intent-to-treat analysis, with missing values considered as failures.
b
Number of patients evaluable.
c
PI major L24I, D30N, V32I, L33F, M46IL, I47AV, G48V, I50LV, F53LY,I54ALMSTV, L76V, V82AFLST,
I84V, N88DS, L90M; PI minor: L10CFIRV, V11I, E35G, K43T, Q58E, A71ILTV, G73ACST, T74P, N83D,
L89V.
d
Includes patients with baseline resistance data.
NA = not applicable.
Data in the paediatric population are very limited. Available data do suggest that atazanavir in
combination with ritonavir may not be effective in treatment experienced children even with very few
(<3) PI mutations.
5.2 Pharmacokinetic properties
The pharmacokinetics of atazanavir were evaluated in healthy adult volunteers and in HIV-infected
patients; significant differences were observed between the two groups. The pharmacokinetics of
atazanavir exhibit a non-linear disposition. In healthy subjects, the AUC of atazanavir from the capsules
and oral powder were similar.
Absorption:
in HIV-infected patients (n=33, combined studies), multiple dosing of REYATAZ 300 mg
once daily with ritonavir 100 mg once daily with food produced a geometric mean (CV%) for
atazanavir, C
max
of 4466 (42%) ng/ml, with time to C
max
of approximately 2.5 hours. The geometric
mean (CV%) for atazanavir C
min
and AUC was 654 (76%) ng/ml and 44185 (51%) ng•h/ml,
respectively.
Food effect:
co-administration of REYATAZ and ritonavir with food optimises the bioavailability of
atazanavir. Co-administration of a single 300-mg dose of REYATAZ and 100-mg dose of ritonavir
with a light meal resulted in a 33% increase in the AUC and a 40% increase in both the C
max
and the
24-hour concentration of atazanavir relative to the fasting state. Co-administration with a high-fat meal
did not affect the AUC of atazanavir relative to fasting conditions and the C
max
was within 11% of
fasting values. The 24-hour concentration following a high fat meal was increased by approximately
33% due to delayed absorption; the median T
max
increased from 2.0 to 5.0 hours. Administration of
REYATAZ with ritonavir with either a light or a high-fat meal decreased the coefficient of variation


























of AUC and C
max
by approximately 25% compared to the fasting state. To enhance bioavailability and
minimise variability, REYATAZ is to be taken with food.
Distribution:
atazanavir was approximately 86% bound to human serum proteins over a concentration
range of 100 to 10,000 ng/ml. Atazanavir binds to both alpha-1-acid glycoprotein (AAG) and albumin
to a similar extent (89% and 86%, respectively, at 1,000 ng/ml). In a multiple-dose study in
HIV-infected patients dosed with 400 mg of atazanavir once daily with a light meal for 12 weeks,
atazanavir was detected in the cerebrospinal fluid and semen.
Metabolism:
studies in humans and
in vitro
studies using human liver microsomes have demonstrated
that atazanavir is principally metabolised by CYP3A4 isozyme to oxygenated metabolites.
Metabolites
are then excreted in the bile as either free or glucuronidated metabolites. Additional minor metabolic
pathways consist of N-dealkylation and hydrolysis. Two minor metabolites of atazanavir in plasma
have been characterised. Neither metabolite demonstrated
in vitro
antiviral activity.
Elimination:
following a single 400-mg dose of
14
C-atazanavir, 79% and 13% of the total radioactivity
was recovered in the faeces and urine, respectively. Unchanged drug accounted for approximately
20% and 7% of the administered dose in the faeces and urine, respectively. Mean urinary excretion of
unchanged drug was 7% following 2 weeks of dosing at 800 mg once daily. In HIV-infected adult
patients (n=33, combined studies) the mean half-life within a dosing interval for atazanavir was 12
hours at steady state following a dose of 300 mg daily with ritonavir 100 mg once daily with a light
meal.
Paediatric patients:
The pharmacokinetics of atazanavir in paediatric patients exhibit an increased
absorption rate compared to adults. There is a slight trend toward a higher clearance in younger
children when normalised for body weight. As a result, greater peak to trough ratios are observed. The
geometric mean AUC values in paediatric patients at recommended doses are expected to be similar to
those observed in adults, with higher geometric mean C
max
(13-17%) and lower geometric mean C
min
(up to 30%) values compared to those in adults. The variability of pharmacokinetic parameters in
younger children is higher.
Impaired renal function
: in healthy subjects, the renal elimination of unchanged atazanavir was
approximately 7% of the administered dose. There are no pharmacokinetic data available for
REYATAZ with ritonavir in patients with renal insufficiency. REYATAZ (without ritonavir) has been
studied in adult patients with severe renal impairment (n=20), including those on haemodialysis, at
multiple doses of 400 mg once daily. Although this study presented some limitations (i.e., unbound
drug concentrations not studied), results suggested that the atazanavir pharmacokinetic parameters
were decreased by 30% to 50% in patients undergoing haemodialysis compared to patients with
normal renal function. The mechanism of this decrease is unknown. (See sections 4.2 and 4.4.)
Impaired hepatic function
: atazanavir is metabolised and eliminated primarily by the liver. The effects
of hepatic impairment on the pharmacokinetics of atazanavir after a 300 mg dose with ritonavir have
not been studied. Concentrations of atazanavir with or without ritonavir are expected to be increased in
patients with moderately or severely impaired hepatic function (see sections 4.2, 4.3, and 4.4).
Age/Gender:
a study of the pharmacokinetics of atazanavir was performed in 59 healthy male and
female subjects (29 young, 30 elderly). There were no clinically important pharmacokinetic
differences based on age or gender.
Race:
a population pharmacokinetic analysis of samples from Phase II clinical trials indicated no
effect of race on the pharmacokinetics of atazanavir.
5.3 Preclinical safety data
In repeat-dose toxicity studies, conducted in mice, rats, and dogs, atazanavir-related findings were
generally confined to the liver and included generally minimal to mild increases in serum bilirubin and
liver enzymes, hepatocellular vacuolation and hypertrophy, and, in female mice only, hepatic
single-cell necrosis. Systemic exposures of atazanavir in mice (males), rats, and dogs at doses
associated with hepatic changes were at least equal to that observed in humans given 400 mg once
daily. In female mice, atazanavir exposure at a dose that produced single-cell necrosis was 12 times
the exposure in humans given 400 mg once daily. Serum cholesterol and glucose were minimally to
mildly increased in rats but not in mice or dogs.
During in vitro studies, cloned human cardiac potassium channel (hERG), was inhibited by 15% at a
concentration (30 μM) of atazanavir corresponding to 30-fold the free drug concentration at C
max
in
humans. Similar concentrations of atazanavir increased by 13% the action potential duration (APD
90
)
in rabbit Purkinje fibres study. Electrocardiographic changes (sinus bradycardia, prolongation of PR
interval, prolongation of QT interval, and prolongation of QRS complex) were observed only in an
initial 2-week oral toxicity study performed in dogs. Subsequent 9-month oral toxicity studies in dogs
showed no drug-related electrocardiographic changes. The clinical relevance of these non-clinical data
is unknown. Potential cardiac effects of this product in humans cannot be ruled out (see sections 4.4
and 4.8). The potential for PR prolongation should be considered in cases of overdose (see section4.9).
In a fertility and early embryonic development study in rats, atazanavir altered oestrus cycling with no
effects on mating or fertility. No teratogenic effects were observed in rats or rabbits at maternally toxic
doses. In pregnant rabbits, gross lesions of the stomach and intestines were observed in dead or
moribund does at maternal doses 2 and 4 times the highest dose administered in the definitive
embryo-development study. In the pre- and postnatal development assessment in rats, atazanavir
produced a transient reduction in body weight in the offspring at a maternally toxic dose. Systemic
exposure to atazanavir at doses that resulted in maternal toxicity was at least equal to or slightly
greater than that observed in humans given 400 mg once daily.
Atazanavir was negative in an Ames reverse-mutation assay but did induce chromosomal aberrations
in vitro
in both the absence and presence of metabolic activation. In
in vivo
studies in rats, atazanavir
did not induce micronuclei in bone marrow, DNA damage in duodenum (comet assay), or unscheduled
DNA repair in liver at plasma and tissue concentrations exceeding those that were clastogenic
in vitro
.
In long-term carcinogenicity studies of atazanavir in mice and rats, an increased incidence of benign
hepatic adenomas was seen in female mice only. The increased incidence of benign hepatic adenomas
in female mice was likely secondary to cytotoxic liver changes manifested by single-cell necrosis and
is considered to have no relevance for humans at intended therapeutic exposures. There were no
tumorigenic findings in male mice or in rats.
Atazanavir increased opacity of bovine corneas in an
in vitro
ocular irritation study, indicating it may
be an ocular irritant upon direct contact with the eye.
PHARMACEUTICAL PARTICULARS
Capsule contents:
Crospovidone
Lactose monohydrate
Magnesium stearate
Capsule shells:
Gelatine
Indigocarmin (E132)
Blue ink containing:
Shellac
Propylene glycol
Ammonium hydroxide
Indigocarmin (E132)
White ink containing:
Shellac
Titanium dioxide (E171)
Ammonium hydroxide
Propylene glycol
Simethicone
6.4 Special precautions for storage
6.5 Nature and contents of container
Each carton contains one high-density polyethylene (HDPE) bottle closed with child-resistant
polypropylene closure. Each bottle contains 60 hard capsules.
Each carton contains 60 x 1 capsules; 10 blister cards of 6 x 1 capsules each in Alu/Alu perforated unit
dose blisters.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal
Any unused product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
BRISTOL-MYERS SQUIBB PHARMA EEIG
Uxbridge Business Park
Sanderson Road
Uxbridge UB8 1DH
United Kingdom
MARKETING AUTHORISATION NUMBER(S)
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 02 March 2004
Date of latest renewal: 02 March 2009
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency (EMEA) http://www.emea.europa.eu
The marketing authorisation holder of REYATAZ is:
BRISTOL-MYERS SQUIBB PHARMA EEIG
Uxbridge Business Park
Sanderson Road
Uxbridge UB8 1DH
United Kingdom
The manufacturer of REYATAZ is:
BRISTOL-MYERS SQUIBB
Champ “Lachaud”, La Goualle
F-19250 Meymac
France
For any further information about this medicine, please contact the local representative of the
Marketing Authorisation Holder:
Belgique/België/Belgien
B
RISTOL
-M
YERS
S
QUIBB
B
ELGIUM
S.A./N.V.
Tél/Tel: + 32 2 352 76 11
Luxembourg/Luxemburg
B
RISTOL
-M
YERS
S
QUIBB
B
ELGIUM
S.A./N.V.
Tél/Tel: + 32 2 352 76 11
България
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Teл.: + 359 800 12 400
Magyarország
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Tel.: + 36 1 301 9700
Česká republika
B
RISTOL
-M
YERS
S
QUIBB SPOL
.
S R
.
O
.
Tel: + 420 221 016 111
Malta
B
RISTOL
-M
YERS
S
QUIBB
S.
R
.
L
.
Tel: + 39 06 50 39 61
Keep out of the reach and sight of children.
Keep the bottle tightly closed.
Danmark
B
RISTOL
-M
YERS
S
QUIBB
Tlf: + 45 45 93 05 06
Nederland
B
RISTOL
-M
YERS
S
QUIBB
BV
Tel: + 31 34 857 42 22
Deutschland
B
RISTOL
-M
YERS
S
QUIBB
G
MB
H
&
C
O
.
KG
A
A
Tel: + 49 89 121 42-0
Norge
B
RISTOL
-M
YERS
S
QUIBB
N
ORWAY
L
TD
Tlf: + 47 67 55 53 50
Eesti
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Tel: + 372 6827 400
Österreich
B
RISTOL
-M
YERS
S
QUIBB
G
ESMB
H
Tel: + 43 1 60 14 30
Ελλάδα
B
RISTOL
-M
YERS
S
QUIBB
A.E.
Τηλ: + 30 210 6074300
Polska
B
RISTOL
-M
YERS
S
QUIBB
P
OLSKA
S
P
.
Z O
.
O
.
Tel.: + 48 22 5796666
España
B
RISTOL
-M
YERS
S
QUIBB
,
S.A.
Tel: + 34 91 456 53 00
Portugal
B
RISTOL
-M
YERS
S
QUIBB
F
ARMACÊUTICA
P
ORTUGUESA
, S.A.
Tel: + 351 21 440 70 00
France
B
RISTOL
-M
YERS
S
QUIBB
S
ARL
Tél: + 33 (0)810 410 500
România
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Tel: + 40 (0)21 272 16 00
Ireland
B
RISTOL
-M
YERS
S
QUIBB
P
HARMACEUTICALS
L
TD
Tel: + 353 (1 800) 749 749
Slovenija
B
RISTOL
-M
YERS
S
QUIBB SPOL
.
S R
.
O
.
Tel: + 386 1 236 47 00
Ísland
V
ISTOR HF
Sími: + 354 535 7000
Slovenská republika
B
RISTOL
-M
YERS
S
QUIBB SPOL
.
S R
.
O
.
Tel: + 421 2 59298411
Italia
B
RISTOL
-M
YERS
S
QUIBB
S.
R
.
L
.
Tel: + 39 06 50 39 61
Suomi/Finland
O
Y
B
RISTOL
-M
YERS
S
QUIBB
(F
INLAND
)
A
B
Puh/Tel: + 358 9 251 21 230
Κύπρος
BRISTOL-MYERS
SQUIBB
A.E
Τηλ: + 357 800 92666
Sverige
B
RISTOL
-M
YERS
S
QUIBB
AB
Tel: + 46 8 704 71 00
Latvija
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Tel: + 371 67 50 21 85
United Kingdom
B
RISTOL
-M
YERS
S
QUIBB
P
HARMACEUTICALS
L
TD
Tel: + 44 (0800) 731 1736
Lietuva
B
RISTOL
-M
YERS
S
QUIBB
G
YÓGYSZERKERESKEDELMI
K
FT
.
Tel: + 370 5 2790 762
This leaflet was last approved in
Detailed information on this medicine is available on the European Medicines Agency (EMEA) web
site: http://www.emea.europa.eu/.

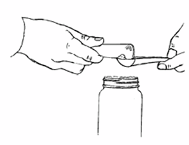
Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/reyataz.html
Copyright © 1995-2021 ITA all rights reserved.
|


















































































































































































































































































































































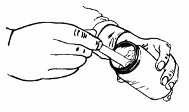

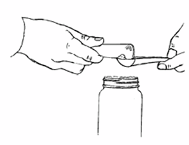
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































