Product Characteristics
ANNEX I
SUMMARY OF PRODUCT CHARACTERISTICS
NAME OF THE MEDICINAL PRODUCT
Temodal 5 mg hard capsules
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each hard capsule contains 5 mg temozolomide.
Excipient: Each hard capsule contains 132.8 mg of anhydrous lactose.
For a full list of excipients, see section 6.1.
The hard capsules have an opaque white body, an opaque green cap, and are imprinted with black ink.
The cap is imprinted with “Temodal”. The body is imprinted with "5 mg", the Schering-Plough logo and
two stripes.
4.1 Therapeutic indications
Temodal hard capsules is indicated for the treatment of:
-
adult patients with newly-diagnosed glioblastoma multiforme concomitantly with radiotherapy
(RT) and subsequently as monotherapy treatment.
children from the age of three years, adolescents and adult patients with malignant glioma, such
as glioblastoma multiforme or anaplastic astrocytoma, showing recurrence or progression after
standard therapy.
4.2 Posology and method of administration
Temodal hard capsules should only be prescribed by physicians experienced in the oncological
treatment of brain tumours.
Anti-emetic therapy may be administered (see section 4.4).
Adult patients with newly-diagnosed glioblastoma multiforme
Temodal hard capsules is administered in combination with focal radiotherapy (concomitant phase)
followed by up to 6 cycles of temozolomide (TMZ) monotherapy (monotherapy phase).
Concomitant phase
TMZ is administered orally at a dose of 75 mg/m
2
daily for 42 days concomitant with focal radiotherapy
(60 Gy administered in 30 fractions). No dose reductionsare recommended, but delay or discontinuation
of TMZ administration should be decided weekly according to haematological and non-haematological
toxicity criteria. TMZ administration can be continued throughout the 42 day concomitant period (up to
49 days) if all of the following conditions are met:
-
absolute neutrophil count (ANC) ≥ 1.5 x 10
9
/l
-
thrombocyte count ≥ 100 x 10
9
/l
-
common toxicity criteria (CTC) non-haematological toxicity ≤ Grade 1 (except for alopecia, nausea
and vomiting).
During treatment a complete blood count should be obtained weekly. TMZ administration should be
temporarily interrupted or permanently discontinued during the concomitant phase according to the
haematological and non-haematological toxicity criteria as noted in Table 1.
Table 1. TMZ dosing interruption or discontinuation during
concomitant radiotherapy and TMZ
Absolute neutrophil count
≥ 0.5 and < 1.5 x 10
9
/l
CTC non-haematological toxicity
(except for alopecia, nausea,
vomiting)
a: Treatment with concomitant TMZ can be continued when all of the following conditions are met:
absolute neutrophil count ≥ 1.5
x 10
9
/l; thrombocyte count ≥ 100
x 10
9
/l; CTC non-haematological
toxicity ≤ Grade 1 (except for alopecia, nausea, vomiting).
Four weeks after completing the TMZ + RT concomitant phase, TMZ is administered for up to 6 cycles
of monotherapy treatment. Dose in Cycle 1 (monotherapy) is 150 mg/m
2
once daily for 5 days followed
by 23 days without treatment. At the start of Cycle 2, the dose is escalated to 200 mg/m
2
if the CTC non-
haematological toxicity for Cycle 1 is Grade ≤ 2 (except for alopecia, nausea and vomiting), absolute
neutrophil count (ANC) is ≥ 1.5 x 10
9
/l, and the thrombocyte count is ≥ 100 x 10
9
/l. If the dose was not
escalated at Cycle 2, escalation should not be done in subsequent cycles. Once escalated, the dose
remains at 200 mg/m
2
per day for the first 5 days of each subsequent cycle except if toxicity occurs.
Dose reductions and discontinuations during the monotherapy phase should be applied according to
Tables 2 and 3.
During treatment a complete blood count should be obtained on Day 22 (21 days after the first dose of
TMZ). The dose should be reduced or administration discontinued according to Table 3.
TMZ dose levels for monotherapy treatment
Reduction for prior toxicity
Dose during Cycles 2-6 in absence of toxicity
Table 3. TMZ dose reduction or discontinuation during monotherapy treatment
Toxicity
Reduce TMZ by 1 dose
level
a
Absolute neutrophil count
CTC non-haematological Toxicity
(except for alopecia, nausea, vomiting)
CTC Grade 3
a: TMZ dose levels are listed in Table 2.
b: TMZ is to be discontinued if:
•
dose level -1 (100 mg/m
2
) still results in unacceptable toxicity
•
the same Grade 3 non-haematological toxicity (except for alopecia, nausea, vomiting) recurs after dose
reduction.


























Adult and paediatric patients 3 years of age or older with recurrent or progressive malignant glioma
:
A treatment cycle comprises 28 days. In patients previously untreated with chemotherapy, TMZ is
administered orally at a dose of 200 mg/m
2
once daily for the first 5 days followed by a 23 day
treatment interruption (total of 28 days). In patients previously treated with chemotherapy, the initial
dose is 150 mg/m
2
once
daily, to be increased in the second cycle to 200 mg/m
2
once daily, for 5 days if
there is no haematological toxicity (see section 4.4)
In patients 3 years of age or older, TMZ is only to be used in recurrent or progressive malignant glioma.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children is very limited (see sections 4.4 and 5.1).
Patients with hepatic or renal impairment
The pharmacokinetics of TMZ were comparable in patients with normal hepatic function and in those
with mild or moderate hepaticimpairment. No data are available on the administration of TMZ in
patients with severe hepatic impairment (Child’s Class C) or with renalimpairment. Based on the
pharmacokinetic properties of TMZ, it is unlikely that dose reductions are required in patients with
severe hepatic impairment or any degree of renalimpairment. However, caution should be exercised
when TMZ is administered in these patients.
Based on a population pharmacokinetic analysis in patients 19-78 years of age, clearance of TMZ is not
affected by age. However, elderly patients (> 70 years of age) appear to be at increased risk of
neutropenia and thrombocytopenia (see section 4.4).
Temodal hard capsules should be administered in the fasting state.
The capsules must be swallowed whole with a glass of water and must not be opened or chewed.
If vomiting occurs after the dose is administered, a second dose should not be administered that day.
Hypersensitivity to the active substanceor to any of the excipients.
Hypersensitivity to dacarbazine (DTIC).
Severe myelosuppression (see section 4.4).
4.4 Special warnings and precautions for use
Pneumocystis carinii
pneumonia
Patients who received concomitant TMZ and RT in a pilot trial for the prolonged 42-day schedule were
shown to be at particular risk for developing
Pneumocystis carinii
pneumonia (PCP). Thus, prophylaxis
against PCP is required for all patients receiving concomitant TMZ and RT for the 42-day regimen
(with a maximum of 49 days) regardless of lymphocyte count. If lymphopenia occurs, they are to
continue the prophylaxis until recovery of lymphopenia to grade ≤ 1.
There may be a higher occurrence of PCP when TMZ is administered during a longer dosing regimen.
However, all patients receiving TMZ, particularly patients receiving steroids, should be observed
closely for the development of PCP, regardless of the regimen.
Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukaemia, have
also been reported very rarely (see section 4.8).
Nausea and vomiting are very commonly associated with TMZ.
Anti-emetic therapy may be administered prior to or following administration of TMZ.
Adult patients with newly-diagnosed glioblastoma multiforme
Anti-emetic prophylaxis is recommended prior to the initial dose of concomitant phase and it is strongly
recommended during the monotherapy phase.
Patients with recurrent or progressive malignant glioma
Patients who have experienced severe (Grade 3 or 4) vomiting in previous treatment cycles may require
anti-emetic therapy.
Prior to dosing, the following laboratory parameters must be met: ANC ≥ 1.5 x 10
9
/l and platelet count
≥ 100 x 10
9
/l. A complete blood count should be obtained on Day 22 (21 days after the first dose) or
within 48 hours of that day, and weekly until ANC > 1.5 x 10
9
/l and platelet count > 100 x 10
9
/l. If
ANC falls to < 1.0 x 10
9
/l or the platelet count is < 50 x 10
9
/l during any cycle, the next cycle should be
reduced one dose level (see section 4.2). Dose levels include 100 mg/m
2
, 150 mg/m
2
, and 200 mg/m
2
.
The lowest recommended dose is 100 mg/m
2
.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children and adolescents is very limited (see sections 4.2 and 5.1).
Elderly patients (> 70 years of age)
Elderly patients appear to be at increased risk of neutropenia and thrombocytopenia, compared with
younger patients. Therefore, special care should be taken when TMZ is administered in elderly patients.
Men being treated with TMZ should be advised not to father a child up to 6 months after receiving the
last dose and to seek advice on cryoconservation of sperm prior to treatment (see section 4.6).
This medicinal product contains lactose. Patients with rare hereditary problems of galactose intolerance,
the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
4.5 Interaction with other medicinal products and other forms of interaction
Interaction studies have only been performed in adults.
In a separate phase I study, administration of TMZ with ranitidine did not result in alterations in the
extent of absorption of temozolomide or the exposure to its active metabolite monomethyl
triazenoimidazole carboxamide (MTIC).
Administration of TMZ with food resulted in a 33 % decrease in C
max
and a 9 % decrease in area under
the curve (AUC).
As it cannot be excluded that the change in C
max
is clinically significant, Temodal should be
administered without food.
Based on an analysis of population pharmacokinetics in phase II trials, co-administration of
dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, H
2
receptor antagonists, or
phenobarbital did not alter the clearance of TMZ. Co-administration with valproic acid was associated
with a small but statistically significant decrease in clearance of TMZ.
No studies have been conducted to determine the effect of TMZ on the metabolism or elimination of
other medicinal products. However, since TMZ does not undergo hepatic metabolism and exhibits low
protein binding, it is unlikely that it would affect the pharmacokinetics of other medicinal products (see
section 5.2).
Use of TMZ in combination with other myelosuppressive agents may increase the likelihood of
myelosuppression.
4.6 Pregnancy and lactation
There are no data in pregnant women. In preclinical studies in rats and rabbits receiving 150 mg/m
2
TMZ, teratogenicity and/or foetal toxicity were demonstrated (see section 5.3). Temodal hard capsules
should not be administered to pregnant women. If use during pregnancy must be considered, the patient
should be apprised of the potential risk to the foetus. Women of childbearing potential should be
advised to use effective contraception to avoid pregnancy while they are receiving TMZ.
It is not known whether TMZ is excreted in human milk; thus, breast-feeding should be discontinued
while receiving treatment with TMZ.
TMZ can have genotoxic effects. Therefore, men being treated with it should be advised not to father a
child up to 6 months after receiving the last dose and to seek advice on cryoconservation of sperm prior
to treatment, because of the possibility of irreversible infertility due to therapy with TMZ.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. The ability to
drive and use machines may be impaired in patients treated with TMZ due to fatigue and somnolence.
Clinical trial experience
In patients treated with TMZ, whether used in combination with RT or as monotherapy following RT
for newly-diagnosed glioblastoma multiforme, or as monotherapy in patients with recurrent or
progressive glioma, the reported very common adverse reactions were similar: nausea, vomiting,
constipation, anorexia, headache and fatigue. Convulsions were reported very commonly in the newly-
diagnosed glioblastoma multiforme patients receiving monotherapy, and rash was reported very
commonly in newly-diagnosed glioblastoma multiforme patients receiving TMZ concurrent with RT
and also as monotherapy, and commonly in recurrent glioma. Most haematologic adverse reactions were
reported commonly or very commonly in both indications (Tables 4 and 5);the frequency of grade 3-4
laboratory findings is presented after each table.
In the tables undesirable effects are classified according to System Organ Class and frequency.
Frequency groupings are defined according to the following convention: Very common (≥ 1/10);
Common (≥ 1/100 to < 1/10); Uncommon (≥ 1/1,000 to < 1/100). Within each frequency grouping,
undesirable effects are presented in order of decreasing seriousness.
Newly-diagnosed glioblastoma multiforme
Table 4 provides treatment-emergent adverse events in patients with newly-diagnosed glioblastoma
multiforme during the concomitant and monotherapy phases of treatment.
Table 4. Treatment-emergent events during concomitant and monotherapy treatment phases
in patients with newly-diagnosed glioblastoma multiforme
TMZ + concomitant RT
n=288*
Infections and infestations
Common:
Infection
, Herpes
simplex
, wound
infection, pharyngitis, candidiasis oral
Infection, candidiasis oral
Herpes simplex
, herpes zoster,
influenza–like symptoms
Blood and lymphatic system disorders
Common:
Neutropenia, thrombocytopenia,
lymphopenia, leukopenia
Febril neutropenia,
thrombocytopenia, anaemia,
leukopenia
Febrile neutropenia, anaemia
Endocrine disorders
Uncommon:
Metabolism and nutrition disorders
Very common:
Hyperglycaemia, weight decreased
Hypokalemia, alkaline phosphatase
increased, weight increased
Hyperglycaemia, weight increased
Psychiatric disorders
Common:
Anxiety, emotional lability, insomnia
Anxiety, depression, emotional
lability, insomnia
Agitation, apathy, behaviour disorder,
depression, hallucination
Nervous system disorders
Very common:





















Convulsions, consciousness decreased,
somnolence, aphasia, balance impaired,
dizziness, confusion, memory
impairment, concentration impaired,
neuropathy, paresthesia, speech disorder,
tremor
Hemiparesis, aphasia, balance
impaired, somnolence, confusion,
dizziness, memory impairment,
concentration impaired, dysphasia,
neurological disorder (NOS),
neuropathy, peripheral neuropathy,
paresthesia, speech disorder, tremor
Status epilepticus, extrapyramidal
disorder, hemiparesis, ataxia, cognition
impaired, dysphasia, gait abnormal,
hyperesthesia, hypoesthesia, neurological
disorder (NOS), peripheral neuropathy
Hemiplegia, ataxia, coordination
abnormal, gait abnormal,
hyperesthesia, sensory disturbance
Visual field defect, vision blurred,
diplopia
Hemianopia, visual acuity reduced, vision
disorder, visual field defect, eye pain
Visual acuity reduced, eye pain, eyes
dry
Ear and labyrinth disorders
Hearing impairment, tinnitus
Otitis media, tinnitus, hyperacusis,
earache
Deafness, vertigo, earache
Vascular disorders
Common:
Haemorrhage, oedema, oedema leg
Haemorrhage, deep venous
thrombosis, oedema leg
Cerebral haemorrhage, hypertension
Embolism pulmonary, oedema,
oedema peripheral
Respiratory, thoracic and mediastinal disorders
Pneumonia, upper respiratory infection,
nasal congestion
Pneumonia, sinusitis, upper
respiratory infection, bronchitis
Gastrointestinal disorders
Constipation, nausea, vomiting
Constipation, nausea, vomiting
Stomatitis, diarrhoea, abdominal pain,
dyspepsia, dysphagia
Stomatitis, diarrhoea, dyspepsia,
dysphagia, mouth dry
Abdominal distension, fecal
incontinence, gastrointestinal disorder
(NOS), gastroenteritis, haemorrhoids
Skin and subcutaneous tissue disorders
























Dermatitis, dry skin, erythema, pruritus
Skin exfoliation, photosensitivity
reaction, pigmentation abnormal
Erythema, pigmentation abnormal,
sweating increased
Musculoskeletal and connective tissue disorders
Common:
Muscle weakness, arthralgia
Muscle weakness, arthralgia,
musculoskeletal pain, myalgia
Myopathy, back pain, musculoskeletal
pain, myalgia
Renal and urinary disorders
Common:
Micturition frequency, urinary
incontinence
Reproductive system and breast disorders
Uncommon:
Vaginal haemorrhage, menorrhagia,
amenorrhea, vaginitis, breast pain
General disorders and administration site conditions
Very common:
Allergic reaction, fever, radiation injury,
face oedema, pain, taste perversion
Allergic reaction, fever, radiation
injury, pain, taste perversion
Asthenia, flushing, hot flushes, condition
aggravated, rigors, tongue discolouration,
parosmia, thirst
Asthenia, face oedema, pain,
condition aggravated, rigors, tooth
disorder, taste perversion
Hepatic enzymes increased, Gamma GT
increased, AST increased
*A patient who was randomised to the RT arm only, received TMZ + RT.
Myelosuppression (neutropenia and thrombocytopenia), which is known dose-limiting toxicity for most
cytotoxic agents, including TMZ, was observed. When laboratory abnormalities and adverse events
were combined across concomitant and monotherapy treatment phases, Grade 3 or Grade 4 neutrophil
abnormalities including neutropenic events were observed in 8 % of the patients. Grade 3 or Grade 4
thrombocyte abnormalities, including thrombocytopenic events were observed in 14 % of the patients
who received TMZ.
Recurrent or progressive malignant glioma
In clinical trials, the most frequently occurring treatment-related undesirable effects were
gastrointestinal disorders, specifically nausea (43 %) and vomiting (36 %). These reactions were usually





















Grade 1 or 2 (0 – 5 episodes of vomiting in 24 hours) and were either self-limiting or readily controlled
with standard anti-emetic therapy. The incidence of severe nausea and vomiting was 4 %.
Table 5 includes adverse reactions reported during clinical trials for recurrent or progressive malignant
glioma and following the marketing of Temodal.
Table 5. Adverse reactions in patients with recurrent or progressive malignant glioma
Infections and infestations
Rare:
Opportunistic infections, including PCP
Blood and lymphatic system disorders
Very common:
Neutropenia or lymphopenia (grade 3-4),
thrombocytopenia (grade 3-4)
Pancytopenia, anaemia (grade 3-4), leukopenia
Metabolism and nutrition disorders
Very common:
Nervous system disorders
Very common:
Somnolence, dizziness, paresthesia
Respiratory, thoracic and mediastinal disorders
Common:
Gastrointestinal disorders
Very common:
Vomiting, nausea, constipation
Diarrhoea, abdominal pain, dyspepsia
Skin and subcutaneous tissue disorders
Common:
Erythema multiforme, erythroderma, urticaria,
exanthema
General disorders and administration site conditions
Very common:
Fever, asthenia, rigors, malaise, pain, taste perversion
Allergic reactions, including anaphylaxis, angioedema
Grade 3 or 4 thrombocytopenia and neutropenia occurred in 19 % and 17 % respectively, of patients
treated for malignant glioma. This led to hospitalisation and/or discontinuation of TMZ in 8 % and 4 %,
respectively. Myelosuppression was predictable (usually within the first few cycles, with the nadir
between Day 21 and Day 28), and recovery was rapid, usually within 1-2 weeks. No evidence of
cumulative myelosuppression was observed. The presence of thrombocytopenia may increase the risk of
bleeding, and the presence of neutropenia or leukopenia may increase the risk of infection.
In a population pharmacokinetics analysis of clinical trial experience there were 101 female and
169 male subjects for whom nadir neutrophil counts were available and 110 female and 174 male
subjects for whom nadir platelet counts were available. There were higher rates of Grade 4 neutropenia
(ANC < 0.5 x 10
9
/l), 12 %
vs
5 %, and thrombocytopenia (< 20 x 10
9
/l ), 9 %
vs
3 %, in women
vs
men
in the first cycle of therapy. In a 400 subject recurrent glioma data set, Grade 4 neutropenia occurred in
8 % of female
vs
4 % of male subjects and Grade 4 thrombocytopenia in 8 % of female
vs
3 % of male



























subjects in the first cycle of therapy. In a study of 288 subjects with newly-diagnosed glioblastoma
multiforme, Grade 4 neutropenia occurred in 3 % of female
vs
0 % of male subjects and Grade 4
thrombocytopenia in 1 % of female
vs
0 % of male subjects in the first cycle of therapy.
Post-Marketing Experience
Antineoplastic agents, and notably alkylating agents, have been associated with a potential risk of
myelodysplastic syndrome (MDS) and secondary malignancies, including leukaemia. Very rare cases of
MDS and secondary malignancies, including myeloid leukaemia have been reported in patients treated
with regimens that included TMZ. Prolonged pancytopenia, which may result in aplastic anaemia has
been reported very rarely
.
Cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported very rarely.
Cases of interstitial pneumonitis/pneumonitis have been reported very rarely.
Doses of 500, 750, 1,000, and 1,250 mg/m
2
(total dose per cycle over 5 days) have been evaluated
clinically in patients. Dose-limiting toxicity was haematological and was reported with any dose but is
expected to be more severe at higher doses. An overdose of 10,000 mg (total dose in a single cycle, over
5 days) was taken by one patient and the adverse reactions reported were pancytopenia, pyrexia, multi-
organ failure and death. There are reports of patients who have taken the recommended dose for more
than 5 days of treatment (up to 64 days) with adverse events reported including bone marrow
suppression, with or without infection, in some cases severe and prolonged and resulting in death. In the
event of an overdose, haematological evaluation is needed. Supportive measures should be provided as
necessary.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group:
Antineoplastic agents - Other alkylating agents, ATC code: L01A X03
Temozolomide is a triazene, which undergoes rapid chemical conversion at physiologic pH to the active
monomethyl triazenoimidazole carboxamide (MTIC). The cytotoxicity of MTIC is thought to be due
primarily to alkylation at the O
6
position of guanine with additional alkylation also occurring at the N
7
position. Cytotoxic lesions that develop subsequently are thought to involve aberrant repair of the
methyl adduct.
Newly-diagnosed glioblastoma multiforme
A total of 573 patients were randomised to receive either TMZ + RT (n=287) or RT alone (n=286).
Patients in the TMZ + RT arm received concomitant TMZ (75 mg/m
2
) once daily, starting the first day
of RT until the last day of RT, for 42 days (with a maximum of 49 days). This was followed by
monotherapy TMZ (150 - 200 mg/m
2
) on Days 1 - 5 of every 28-day cycle for up to 6 cycles, starting
4 weeks after the end of RT. Patients in the control arm received RT only.
Pneumocystis carinii
pneumonia (PCP) prophylaxis was required during RT and combined TMZ therapy.
TMZ was administered as salvage therapy in the follow-up phase in 161 patients of the 282 (57 %) in
the RT alone arm, and 62 patients of the 277 (22 %) in the TMZ + RT arm.
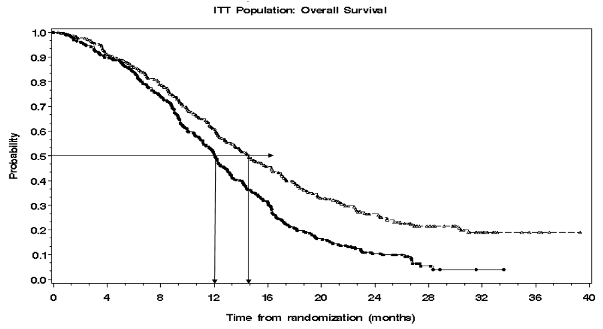
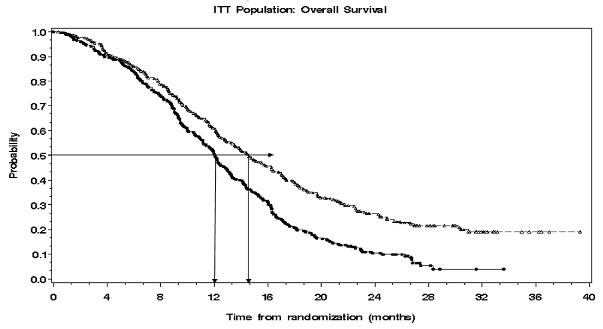
The hazard ratio (HR) for overall survival was 1.59 (95 % CI for HR=1.33 -1.91) with a log-rank
p < 0.0001 in favour of the TMZ arm. The estimated probability of surviving 2 years or more (26 %
vs
10 %) is higher for the RT + TMZ arm. The addition of concomitant TMZ to RT, followed by TMZ
monotherapy in the treatment of patients with newly-diagnosed glioblastoma multiforme demonstrated a
statistically significant improvement in overall survival (OS) compared with RT alone (Figure 1).
HR (95% C.I.) = 1.59 (1.33 – 1.91)
log-rank p-value < .0001
Kaplan-Meier curves for overall survival (intent-to-treat population)
The results from the trial were not consistent in the subgroup of patients with a poor performance status
(WHO PS=2, n=70), where overall survival and time to progression were similar in both arms.
However, no unacceptable risks appear to be present in this patient group.
Recurrent or progressive malignant glioma
Data on clinical efficacy in patients with glioblastoma multiforme (Karnofsky performance status [KPS]
≥ 70), progressive or recurrent after surgery and RT, were based on two clinical trials with oral TMZ.
One was a non-comparative trial in 138 patients (29 % received prior chemotherapy), and the other was
a randomised active-controlled trial of TMZ
vs
procarbazine in a total of 225 patients (67 % received
prior treatment with nitrosourea based chemotherapy). In both trials, the primary endpoint was
progression-free survival (PFS) defined by MRI scans or neurological worsening. In the non-
comparative trial, the PFS at 6 months was 19 %, the median progression-free survival was 2.1 months,
and the median overall survival 5.4 months. The objective response rate (ORR) based on MRI scans was
8 %.
In the randomised active-controlled trial, the PFS at 6 months was significantly greater for TMZ than for
procarbazine (21 %
vs
8 %, respectively – chi-square p = 0.008) with median PFS of 2.89 and
1.88 months respectively (log rank p = 0.0063). The median survival was 7.34 and 5.66 months for TMZ
and procarbazine, respectively (log rank p = 0.33). At 6 months, the fraction of surviving patients was
significantly higher in the TMZ arm (60 %) compared with the procarbazine arm (44 %) (chi-square
p = 0.019). In patients with prior chemotherapy a benefit was indicated in those with a KPS ≥ 80.
Data on time to worsening of neurological status favoured TMZ over procarbazine as did data on time
to worsening of performance status (decrease to a KPS of < 70 or a decrease by at least 30 points). The
median times to progression in these endpoints ranged from 0.7 to 2.1 months longer for TMZ than for
procarbazine (log rank p = < 0.01 to 0.03).

Recurrent anaplastic astrocytoma
In a multicentre, prospective phase II trial evaluating the safety and efficacy of oral TMZ in the
treatment of patients with anaplastic astrocytoma at first relapse, the 6 month PFS was 46 %. The
median PFS was 5.4 months. Median overall survival was 14.6 months. Response rate, based on the
central reviewer assessment, was 35 % (13 CR and 43 PR) for the intent-to-treat population (ITT)
n=162. In 43 patients stable disease was reported. The 6-month event-free survival for the ITT
population was 44 % with a median event-free survival of 4.6 months, which was similar to the results
for the progression-free survival. For the eligible histology population, the efficacy results were similar.
Achieving a radiological objective response or maintaining progression-free status was strongly
associated with maintained or improved quality of life.
Oral TMZ has been studied in paediatric patients (age 3-18 years) with recurrent brainstem glioma or
recurrent high grade astrocytoma, in a regimen administered daily for 5 days every 28 days. Tolerance
to TMZ is similar to adults.
5.2 Pharmacokinetic properties
TMZ is spontaneously hydrolyzed at physiologic pH primarily to the active species, 3-methyl-(triazen-
1-yl)imidazole-4-carboxamide (MTIC). MTIC is spontaneously hydrolyzed to 5-amino-imidazole-4-
carboxamide (AIC), a known intermediate in purine and nucleic acid biosynthesis, and to
methylhydrazine, which is believed to be the active alkylating species. The cytotoxicity of MTIC is
thought to be primarily due to alkylation of DNA mainly at the O
6
and N
7
positions of guanine. Relative
to the AUC of TMZ, the exposure to MTIC and AIC is ~ 2.4 % and 23 %, respectively.
In vivo
, the t
1/2
of MTIC was similar to that of TMZ, 1.8 hr.
After oral administration to adult patients, TMZ is absorbed rapidely, with peak concentrations reached
as early as 20 minutes post-administration (mean time between 0.5 and 1.5 hours). After oral
administration of
14
C-labelled TMZ, mean faecal excretion of
14
C over 7 days post-dose was 0.8 %
indicationg complete absorption.
TMZ demonstrates low protein binding (10 % to 20 %), and thus it is not expected to interact with
highly protein-bound substances.
PET studies in humans and preclinical data suggest that TMZ crosses the blood-brain barrier rapidly and
is present in the CSF. CSF penetration was confirmed in one patient; CSF exposure based on AUC of
TMZ was approximately 30 % of that in plasma, which is consistent with animal data.
The half-life (t
1/2
) in plasma is approximately 1.8 hours. The major route of
14
C elimination is renal.
Following oral administration, approximately 5 % to 10 % of the dose is recovered unchanged in the
urine over 24 hours, and the remainder excreted as temozolomide acid, 5-aminoimidazole-4-
carboxamide (AIC) or unidentified polar metabolites.
Plasma concentrations increase in a dose-related manner. Plasma clearance, volume of distribution and
half-life are independent of dose.
Analysis of population-based pharmacokinetics of TMZ revealed that plasma TMZ clearance was
independent of age, renal function
or tobacco use. In a separate pharmacokinetic study, plasma
pharmacokinetic profiles in patients with mild to moderate hepatic impairment were similar to those
observed in patients with normal hepatic function.
Paediatric patients had a higher AUC than adult patients; however, the maximum tolerated dose (MTD)
was 1,000 mg/m
2
per cycle both in children and in adults.
5.3 Preclinical safety data
Single-cycle (5-day dosing, 23 days non-treatment), 3- and 6-cycle toxicity studies were conducted in
rats and dogs. The primary targets of toxicity included the bone marrow, lymphoreticular system, testes,
the gastrointestinal tract and, at higher doses, which were lethal to 60 % to 100 % of rats and dogs
tested, degeneration of the retina occurred. Most of the toxicity showed evidence of reversibility, except
for adverse events on the male reproductive system and retinal degeneration. However, because the
doses implicated in retinal degeneration were in the lethal dose range, and no comparable effect has
been observed in clinical studies, this finding was not considered to have clinical relevance.
TMZ is an embryotoxic, teratogenic and genotoxic alkylating agent. TMZ is more toxic to the rat and
dog than to humans, and the clinical dose approximates the minimum lethal dose in rats and dogs. Dose-
related reductions in leukocytes and platelets appear to be sensitive indicators of toxicity. A variety of
neoplasms, including mammary carcinomas, keratocanthoma of the skin and basal cell adenoma were
observed in the 6-cycle rat study while no tumours or pre-neoplastic changes were evident in dog
studies. Rats appear to be particularly sensitive to oncogenic effects of TMZ, with the occurrence of first
tumours within 3 months of initiating dosing. This latency period is very short even for an alkylating
agent.
Results of the Ames/salmonella and Human Peripheral Blood Lymphocyte (HPBL) chromosome
aberration tests showed a positive mutagenicity response.
PHARMACEUTICAL PARTICULARS
Capsule content
:
anhydrous lactose,
colloidal anhydrous silica,
sodium starch glycolate type A,
tartaric acid,
stearic acid.
Capsule shell
:
gelatin,
titanium dioxide (E 171),
sodium laurilsulfate,
yellow iron oxide (E 172),
indigo carmine (E 132),
Printing ink:
shellac,
propylene glycol,
purified water,
ammonium hydroxide,
potassium hydroxide,
black iron oxide (E 172).
6.4 Special precautions for storage
Do not store above 30 °C.
Store in the original bottle in order to protect from moisture.
Keep the bottle tightly closed.
Do not store above 30 °C.
6.5 Nature and contents of container
Type I amber glass bottles with polypropylene child-resistant closures containing 5 -or 20 hard capsules.
The carton contains one bottle.
Sachets are composed of linear low density polyethylene (innermost layer), aluminium and polyethylene
terephthalate.
Each sachet contains 1 hard capsule and is dispensed in a cardboard carton.
The carton contains 5 or 20 hard capsules, individually sealed in sachets.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
Capsules should not be opened. If a capsule becomes damaged, contact of the powder contents with skin
or mucous membrane must be avoided. If Temodal comes into contact with skin or mucosa, it should be
washed immediately and thoroughly with soap and water.
Patients should be advised to keep capsules out of the reach and sight of children, preferably in a locked
cupboard. Accidental ingestion can be lethal for children.
Any unused product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
SP Europe
Rue de Stalle 73
B-1180 Bruxelles
Belgium
MARKETING AUTHORISATION NUMBER(S)
EU/1/98/096/001
EU/1/98/096/002
EU/1/98/096/024
EU/1/98/096/025
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 26 January 1999.
Date of last renewal: 26 January 2009
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
NAME OF THE MEDICINAL PRODUCT
Temodal 20 mg hard capsules
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each hard capsule contains 20 mg temozolomide.
Excipient: Each hard capsule contains 182.2 mg of anhydrous lactose.
For a full list of excipients, see section 6.1.
The hard capsules have an opaque white body, an opaque yellow cap, and are imprinted with black ink.
The cap is imprinted with “Temodal”. The body is imprinted with "20 mg", the Schering-Plough logo
and two stripes.
4.1 Therapeutic indications
Temodal hard capsules is indicated for the treatment of:
-
adult patients with newly-diagnosed glioblastoma multiforme concomitantly with radiotherapy
(RT) and subsequently as monotherapy treatment.
children from the age of three years, adolescents and adult patients with malignant glioma, such
as glioblastoma multiforme or anaplastic astrocytoma, showing recurrence or progression after
standard therapy.
4.2 Posology and method of administration
Temodal hard capsules should only be prescribed by physicians experienced in the oncological
treatment of brain tumours.
Anti-emetic therapy may be administered (see section 4.4).
Adult patients with newly-diagnosed glioblastoma multiforme
Temodal hard capsules is administered in combination with focal radiotherapy (concomitant phase)
followed by up to 6 cycles of temozolomide (TMZ) monotherapy (monotherapy phase).
Concomitant phase
TMZ is administered orally at a dose of 75 mg/m
2
daily for 42 days concomitant with focal radiotherapy
(60 Gy administered in 30 fractions). No dose reductionsare recommended, but delay or discontinuation
of TMZ administration should be decided weekly according to haematological and non-haematological
toxicity criteria. TMZ administration can be continued throughout the 42 day concomitant period (up to
49 days) if all of the following conditions are met:
-
absolute neutrophil count (ANC) ≥ 1.5 x 10
9
/l
-
thrombocyte count ≥ 100 x 10
9
/l
-
common toxicity criteria (CTC) non-haematological toxicity ≤ Grade 1 (except for alopecia, nausea
and vomiting).
During treatment a complete blood count should be obtained weekly. TMZ administration should be
temporarily interrupted or permanently discontinued during the concomitant phase according to the
haematological and non-haematological toxicity criteria as noted in Table 1.
Table 1. TMZ dosing interruption or discontinuation during
concomitant radiotherapy and TMZ
Absolute neutrophil count
≥ 0.5 and < 1.5 x 10
9
/l
CTC non-haematological toxicity
(except for alopecia, nausea,
vomiting)
a: Treatment with concomitant TMZ can be continued when all of the following conditions are met:
absolute neutrophil count ≥ 1.5
x 10
9
/l; thrombocyte count ≥ 100
x 10
9
/l; CTC non-haematological
toxicity ≤ Grade 1 (except for alopecia, nausea, vomiting).
Four weeks after completing the TMZ + RT concomitant phase, TMZ is administered for up to 6 cycles
of monotherapy treatment. Dose in Cycle 1 (monotherapy) is 150 mg/m
2
once daily for 5 days followed
by 23 days without treatment. At the start of Cycle 2, the dose is escalated to 200 mg/m
2
if the CTC non-
haematological toxicity for Cycle 1 is Grade ≤ 2 (except for alopecia, nausea and vomiting), absolute
neutrophil count (ANC) is ≥ 1.5 x 10
9
/l, and the thrombocyte count is ≥ 100 x 10
9
/l. If the dose was not
escalated at Cycle 2, escalation should not be done in subsequent cycles. Once escalated, the dose
remains at 200 mg/m
2
per day for the first 5 days of each subsequent cycle except if toxicity occurs.
Dose reductions and discontinuations during the monotherapy phase should be applied according to
Tables 2 and 3.
During treatment a complete blood count should be obtained on Day 22 (21 days after the first dose of
TMZ). The dose should be reduced or administration discontinued according to Table 3.
TMZ dose levels for monotherapy treatment
Reduction for prior toxicity
Dose during Cycles 2-6 in absence of toxicity















Table 3. TMZ dose reduction or discontinuation during monotherapy treatment
Toxicity
Reduce TMZ by 1 dose
level
a
Absolute neutrophil count
CTC non-haematological Toxicity
(except for alopecia, nausea, vomiting)
CTC Grade 3
a: TMZ dose levels are listed in Table 2.
b: TMZ is to be discontinued if:
•
dose level -1 (100 mg/m
2
) still results in unacceptable toxicity
•
the same Grade 3 non-haematological toxicity (except for alopecia, nausea, vomiting) recurs after dose
reduction.
Adult and paediatric patients 3 years of age or older with recurrent or progressive malignant glioma
:
A treatment cycle comprises 28 days. In patients previously untreated with chemotherapy, TMZ is
administered orally at a dose of 200 mg/m
2
once daily for the first 5 days followed by a 23 day
treatment interruption (total of 28 days). In patients previously treated with chemotherapy, the initial
dose is 150 mg/m
2
once
daily, to be increased in the second cycle to 200 mg/m
2
once daily, for 5 days if
there is no haematological toxicity (see section 4.4)
In patients 3 years of age or older, TMZ is only to be used in recurrent or progressive malignant glioma.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children is very limited (see sections 4.4 and 5.1).
Patients with hepatic or renal impairment
The pharmacokinetics of TMZ were comparable in patients with normal hepatic function and in those
with mild or moderate hepaticimpairment. No data are available on the administration of TMZ in
patients with severe hepatic impairment (Child’s Class C) or with renalimpairment. Based on the
pharmacokinetic properties of TMZ, it is unlikely that dose reductions are required in patients with
severe hepatic impairment or any degree of renalimpairment. However, caution should be exercised
when TMZ is administered in these patients.
Based on a population pharmacokinetic analysis in patients 19-78 years of age, clearance of TMZ is not
affected by age. However, elderly patients (> 70 years of age) appear to be at increased risk of
neutropenia and thrombocytopenia (see section 4.4).
Temodal hard capsules should be administered in the fasting state.
The capsules must be swallowed whole with a glass of water and must not be opened or chewed.
If vomiting occurs after the dose is administered, a second dose should not be administered that day.
Hypersensitivity to the active substanceor to any of the excipients.







Hypersensitivity to dacarbazine (DTIC).
Severe myelosuppression (see section 4.4).
4.4 Special warnings and precautions for use
Pneumocystis carinii
pneumonia
Patients who received concomitant TMZ and RT in a pilot trial for the prolonged 42-day schedule were
shown to be at particular risk for developing
Pneumocystis carinii
pneumonia (PCP). Thus, prophylaxis
against PCP is required for all patients receiving concomitant TMZ and RT for the 42-day regimen
(with a maximum of 49 days) regardless of lymphocyte count. If lymphopenia occurs, they are to
continue the prophylaxis until recovery of lymphopenia to grade ≤ 1.
There may be a higher occurrence of PCP when TMZ is administered during a longer dosing regimen.
However, all patients receiving TMZ, particularly patients receiving steroids, should be observed
closely for the development of PCP, regardless of the regimen.
Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukaemia, have
also been reported very rarely (see section 4.8).
Nausea and vomiting are very commonly associated with TMZ.
Anti-emetic therapy may be administered prior to or following administration of TMZ.
Adult patients with newly-diagnosed glioblastoma multiforme
Anti-emetic prophylaxis is recommended prior to the initial dose of concomitant phase and it is strongly
recommended during the monotherapy phase.
Patients with recurrent or progressive malignant glioma
Patients who have experienced severe (Grade 3 or 4) vomiting in previous treatment cycles may require
anti-emetic therapy.
Prior to dosing, the following laboratory parameters must be met: ANC ≥ 1.5 x 10
9
/l and platelet count
≥ 100 x 10
9
/l. A complete blood count should be obtained on Day 22 (21 days after the first dose) or
within 48 hours of that day, and weekly until ANC > 1.5 x 10
9
/l and platelet count > 100 x 10
9
/l. If
ANC falls to < 1.0 x 10
9
/l or the platelet count is < 50 x 10
9
/l during any cycle, the next cycle should be
reduced one dose level (see section 4.2). Dose levels include 100 mg/m
2
, 150 mg/m
2
, and 200 mg/m
2
.
The lowest recommended dose is 100 mg/m
2
.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children and adolescents is very limited (see sections 4.2 and 5.1).
Elderly patients (> 70 years of age)
Elderly patients appear to be at increased risk of neutropenia and thrombocytopenia, compared with
younger patients. Therefore, special care should be taken when TMZ is administered in elderly patients.
Men being treated with TMZ should be advised not to father a child up to 6 months after receiving the
last dose and to seek advice on cryoconservation of sperm prior to treatment (see section 4.6).
This medicinal product contains lactose. Patients with rare hereditary problems of galactose intolerance,
the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
4.5 Interaction with other medicinal products and other forms of interaction
Interaction studies have only been performed in adults.
In a separate phase I study, administration of TMZ with ranitidine did not result in alterations in the
extent of absorption of temozolomide or the exposure to its active metabolite monomethyl
triazenoimidazole carboxamide (MTIC).
Administration of TMZ with food resulted in a 33 % decrease in C
max
and a 9 % decrease in area under
the curve (AUC).
As it cannot be excluded that the change in C
max
is clinically significant, Temodal should be
administered without food.
Based on an analysis of population pharmacokinetics in phase II trials, co-administration of
dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, H
2
receptor antagonists, or
phenobarbital did not alter the clearance of TMZ. Co-administration with valproic acid was associated
with a small but statistically significant decrease in clearance of TMZ.
No studies have been conducted to determine the effect of TMZ on the metabolism or elimination of
other medicinal products. However, since TMZ does not undergo hepatic metabolism and exhibits low
protein binding, it is unlikely that it would affect the pharmacokinetics of other medicinal products (see
section 5.2).
Use of TMZ in combination with other myelosuppressive agents may increase the likelihood of
myelosuppression.
4.6 Pregnancy and lactation
There are no data in pregnant women. In preclinical studies in rats and rabbits receiving 150 mg/m
2
TMZ, teratogenicity and/or foetal toxicity were demonstrated (see section 5.3). Temodal hard capsules
should not be administered to pregnant women. If use during pregnancy must be considered, the patient
should be apprised of the potential risk to the foetus. Women of childbearing potential should be
advised to use effective contraception to avoid pregnancy while they are receiving TMZ.
It is not known whether TMZ is excreted in human milk; thus, breast-feeding should be discontinued
while receiving treatment with TMZ.
TMZ can have genotoxic effects. Therefore, men being treated with it should be advised not to father a
child up to 6 months after receiving the last dose and to seek advice on cryoconservation of sperm prior
to treatment, because of the possibility of irreversible infertility due to therapy with TMZ.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. The ability to
drive and use machines may be impaired in patients treated with TMZ due to fatigue and somnolence.
Clinical trial experience
In patients treated with TMZ, whether used in combination with RT or as monotherapy following RT
for newly-diagnosed glioblastoma multiforme, or as monotherapy in patients with recurrent or
progressive glioma, the reported very common adverse reactions were similar: nausea, vomiting,
constipation, anorexia, headache and fatigue. Convulsions were reported very commonly in the newly-
diagnosed glioblastoma multiforme patients receiving monotherapy, and rash was reported very
commonly in newly-diagnosed glioblastoma multiforme patients receiving TMZ concurrent with RT
and also as monotherapy, and commonly in recurrent glioma. Most haematologic adverse reactions were
reported commonly or very commonly in both indications (Tables 4 and 5);the frequency of grade 3-4
laboratory findings is presented after each table.
In the tables undesirable effects are classified according to System Organ Class and frequency.
Frequency groupings are defined according to the following convention: Very common (≥ 1/10);
Common (≥ 1/100 to < 1/10); Uncommon (≥ 1/1,000 to < 1/100). Within each frequency grouping,
undesirable effects are presented in order of decreasing seriousness.
Newly-diagnosed glioblastoma multiforme
Table 4 provides treatment-emergent adverse events in patients with newly-diagnosed glioblastoma
multiforme during the concomitant and monotherapy phases of treatment.
Table 4. Treatment-emergent events during concomitant and monotherapy treatment phases
in patients with newly-diagnosed glioblastoma multiforme
TMZ + concomitant RT
n=288*
Infections and infestations
Common:
Infection
, Herpes
simplex
, wound
infection, pharyngitis, candidiasis oral
Infection, candidiasis oral
Herpes simplex
, herpes zoster,
influenza–like symptoms
Blood and lymphatic system disorders
Common:
Neutropenia, thrombocytopenia,
lymphopenia, leukopenia
Febril neutropenia,
thrombocytopenia, anaemia,
leukopenia
Febrile neutropenia, anaemia
Endocrine disorders
Uncommon:
Metabolism and nutrition disorders
Very common:
Hyperglycaemia, weight decreased
Hypokalemia, alkaline phosphatase
increased, weight increased
Hyperglycaemia, weight increased
















Psychiatric disorders
Common:
Anxiety, emotional lability, insomnia
Anxiety, depression, emotional
lability, insomnia
Agitation, apathy, behaviour disorder,
depression, hallucination
Nervous system disorders
Very common:
Convulsions, consciousness decreased,
somnolence, aphasia, balance impaired,
dizziness, confusion, memory
impairment, concentration impaired,
neuropathy, paresthesia, speech disorder,
tremor
Hemiparesis, aphasia, balance
impaired, somnolence, confusion,
dizziness, memory impairment,
concentration impaired, dysphasia,
neurological disorder (NOS),
neuropathy, peripheral neuropathy,
paresthesia, speech disorder, tremor
Status epilepticus, extrapyramidal
disorder, hemiparesis, ataxia, cognition
impaired, dysphasia, gait abnormal,
hyperesthesia, hypoesthesia, neurological
disorder (NOS), peripheral neuropathy
Hemiplegia, ataxia, coordination
abnormal, gait abnormal,
hyperesthesia, sensory disturbance
Visual field defect, vision blurred,
diplopia
Hemianopia, visual acuity reduced, vision
disorder, visual field defect, eye pain
Visual acuity reduced, eye pain, eyes
dry
Ear and labyrinth disorders
Hearing impairment, tinnitus
Otitis media, tinnitus, hyperacusis,
earache
Deafness, vertigo, earache
Haemorrhage, oedema, oedema leg
Haemorrhage, deep venous
thrombosis, oedema leg
Cerebral haemorrhage, hypertension
Embolism pulmonary, oedema,
oedema peripheral
Respiratory, thoracic and mediastinal disorders
Pneumonia, upper respiratory infection,
nasal congestion
Pneumonia, sinusitis, upper
respiratory infection, bronchitis
Gastrointestinal disorders
Constipation, nausea, vomiting
Constipation, nausea, vomiting

























Stomatitis, diarrhoea, abdominal pain,
dyspepsia, dysphagia
Stomatitis, diarrhoea, dyspepsia,
dysphagia, mouth dry
Abdominal distension, fecal
incontinence, gastrointestinal disorder
(NOS), gastroenteritis, haemorrhoids
Skin and subcutaneous tissue disorders
Very common:
Dermatitis, dry skin, erythema, pruritus
Skin exfoliation, photosensitivity
reaction, pigmentation abnormal
Erythema, pigmentation abnormal,
sweating increased
Musculoskeletal and connective tissue disorders
Common:
Muscle weakness, arthralgia
Muscle weakness, arthralgia,
musculoskeletal pain, myalgia
Myopathy, back pain, musculoskeletal
pain, myalgia
Renal and urinary disorders
Micturition frequency, urinary
incontinence
Reproductive system and breast disorders
Uncommon:
Vaginal haemorrhage, menorrhagia,
amenorrhea, vaginitis, breast pain
General disorders and administration site conditions
Very common:
Allergic reaction, fever, radiation injury,
face oedema, pain, taste perversion
Allergic reaction, fever, radiation
injury, pain, taste perversion
Asthenia, flushing, hot flushes, condition
aggravated, rigors, tongue discolouration,
parosmia, thirst
Asthenia, face oedema, pain,
condition aggravated, rigors, tooth
disorder, taste perversion
Hepatic enzymes increased, Gamma GT
increased, AST increased
*A patient who was randomised to the RT arm only, received TMZ + RT.
Myelosuppression (neutropenia and thrombocytopenia), which is known dose-limiting toxicity for most
cytotoxic agents, including TMZ, was observed. When laboratory abnormalities and adverse events
were combined across concomitant and monotherapy treatment phases, Grade 3 or Grade 4 neutrophil

























abnormalities including neutropenic events were observed in 8 % of the patients. Grade 3 or Grade 4
thrombocyte abnormalities, including thrombocytopenic events were observed in 14 % of the patients
who received TMZ.
Recurrent or progressive malignant glioma
In clinical trials, the most frequently occurring treatment-related undesirable effects were
gastrointestinal disorders, specifically nausea (43 %) and vomiting (36 %). These reactions were usually
Grade 1 or 2 (0 – 5 episodes of vomiting in 24 hours) and were either self-limiting or readily controlled
with standard anti-emetic therapy. The incidence of severe nausea and vomiting was 4 %.
Table 5 includes adverse reactions reported during clinical trials for recurrent or progressive malignant
glioma and following the marketing of Temodal.
Table 5. Adverse reactions in patients with recurrent or progressive malignant glioma
Infections and infestations
Rare:
Opportunistic infections, including PCP
Blood and lymphatic system disorders
Very common:
Neutropenia or lymphopenia (grade 3-4),
thrombocytopenia (grade 3-4)
Pancytopenia, anaemia (grade 3-4), leukopenia
Metabolism and nutrition disorders
Very common:
Nervous system disorders
Very common:
Somnolence, dizziness, paresthesia
Respiratory, thoracic and mediastinal disorders
Common:
Gastrointestinal disorders
Very common:
Vomiting, nausea, constipation
Diarrhoea, abdominal pain, dyspepsia
Skin and subcutaneous tissue disorders
Common:
Erythema multiforme, erythroderma, urticaria,
exanthema
General disorders and administration site conditions
Very common:
Fever, asthenia, rigors, malaise, pain, taste perversion
Allergic reactions, including anaphylaxis, angioedema
Grade 3 or 4 thrombocytopenia and neutropenia occurred in 19 % and 17 % respectively, of patients
treated for malignant glioma. This led to hospitalisation and/or discontinuation of TMZ in 8 % and 4 %,
respectively. Myelosuppression was predictable (usually within the first few cycles, with the nadir
between Day 21 and Day 28), and recovery was rapid, usually within 1-2 weeks. No evidence of
cumulative myelosuppression was observed. The presence of thrombocytopenia may increase the risk of
bleeding, and the presence of neutropenia or leukopenia may increase the risk of infection.



























In a population pharmacokinetics analysis of clinical trial experience there were 101 female and
169 male subjects for whom nadir neutrophil counts were available and 110 female and 174 male
subjects for whom nadir platelet counts were available. There were higher rates of Grade 4 neutropenia
(ANC < 0.5 x 10
9
/l), 12 %
vs
5 %, and thrombocytopenia (< 20 x 10
9
/l ), 9 %
vs
3 %, in women
vs
men
in the first cycle of therapy. In a 400 subject recurrent glioma data set, Grade 4 neutropenia occurred in
8 % of female
vs
4 % of male subjects and Grade 4 thrombocytopenia in 8 % of female
vs
3 % of male
subjects in the first cycle of therapy. In a study of 288 subjects with newly-diagnosed glioblastoma
multiforme, Grade 4 neutropenia occurred in 3 % of female
vs
0 % of male subjects and Grade 4
thrombocytopenia in 1 % of female
vs
0 % of male subjects in the first cycle of therapy.
Post-Marketing Experience
Antineoplastic agents, and notably alkylating agents, have been associated with a potential risk of
myelodysplastic syndrome (MDS) and secondary malignancies, including leukaemia. Very rare cases of
MDS and secondary malignancies, including myeloid leukaemia have been reported in patients treated
with regimens that included TMZ. Prolonged pancytopenia, which may result in aplastic anaemia has
been reported very rarely
.
Cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported very rarely.
Cases of interstitial pneumonitis/pneumonitis have been reported very rarely.
Doses of 500, 750, 1,000, and 1,250 mg/m
2
(total dose per cycle over 5 days) have been evaluated
clinically in patients. Dose-limiting toxicity was haematological and was reported with any dose but is
expected to be more severe at higher doses. An overdose of 10,000 mg (total dose in a single cycle, over
5 days) was taken by one patient and the adverse reactions reported were pancytopenia, pyrexia, multi-
organ failure and death. There are reports of patients who have taken the recommended dose for more
than 5 days of treatment (up to 64 days) with adverse events reported including bone marrow
suppression, with or without infection, in some cases severe and prolonged and resulting in death. In the
event of an overdose, haematological evaluation is needed. Supportive measures should be provided as
necessary.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group:
Antineoplastic agents - Other alkylating agents, ATC code: L01A X03
Temozolomide is a triazene, which undergoes rapid chemical conversion at physiologic pH to the active
monomethyl triazenoimidazole carboxamide (MTIC). The cytotoxicity of MTIC is thought to be due
primarily to alkylation at the O
6
position of guanine with additional alkylation also occurring at the N
7
position. Cytotoxic lesions that develop subsequently are thought to involve aberrant repair of the
methyl adduct.
Newly-diagnosed glioblastoma multiforme
A total of 573 patients were randomised to receive either TMZ + RT (n=287) or RT alone (n=286).
Patients in the TMZ + RT arm received concomitant TMZ (75 mg/m
2
) once daily, starting the first day
of RT until the last day of RT, for 42 days (with a maximum of 49 days). This was followed by
monotherapy TMZ (150 - 200 mg/m
2
) on Days 1 - 5 of every 28-day cycle for up to 6 cycles, starting
4 weeks after the end of RT. Patients in the control arm received RT only.
Pneumocystis carinii
pneumonia (PCP) prophylaxis was required during RT and combined TMZ therapy.
TMZ was administered as salvage therapy in the follow-up phase in 161 patients of the 282 (57 %) in
the RT alone arm, and 62 patients of the 277 (22 %) in the TMZ + RT arm.
The hazard ratio (HR) for overall survival was 1.59 (95 % CI for HR=1.33 -1.91) with a log-rank
p < 0.0001 in favour of the TMZ arm. The estimated probability of surviving 2 years or more (26 %
vs
10 %) is higher for the RT + TMZ arm. The addition of concomitant TMZ to RT, followed by TMZ
monotherapy in the treatment of patients with newly-diagnosed glioblastoma multiforme demonstrated a
statistically significant improvement in overall survival (OS) compared with RT alone (Figure 1).
HR (95% C.I.) = 1.59 (1.33 – 1.91)
log-rank p-value < .0001
Kaplan-Meier curves for overall survival (intent-to-treat population)
The results from the trial were not consistent in the subgroup of patients with a poor performanc
(WHO PS=2, n=70), where overall survival and time to progression were si
H
owever, no unacceptable risks appear to be present in this patient group.
ecurrent or progressive malignant glioma
Data on clinical efficacy in patients with glioblastoma multiforme (Karnofsky performance status [KPS
≥ 70), progressive or recurrent after surgery and RT, were based on two clinical trials with oral TMZ.
One was a non-comparative trial in 138 patients (29 % received prior chemotherapy), and the other wa
a randomised active-controlled trial of TMZ
vs
procarbazine in a total of 225 patients (67 % rec
prior treatment with nitrosourea based chemotherapy). In both trials, the primary endpoint was
progression-free survival (PFS) defined by MRI scans or neurological worsening. In the non-
comparative trial, the PFS at 6 months was 19 %, the median progression-free survival was 2.1 months,
and th
8
e median overall survival 5.4 months. The objective response rate (ORR) based on MRI scans was
In the randomised active-controlled trial, the PFS at 6 months was significantly greater for TMZ
procarbazine (21 %
vs
8 %, respectively – chi-square p = 0.008) with median PFS of 2.89 and
1.88 months respectively (log rank p = 0.0063). The median survival was 7.34 and 5.66 months for TM
and procarbazine, respectively (log rank p = 0.33). At 6 months, the fraction of surviving patients was
significantly higher in the TMZ arm (60 %) compared with the procarbazine arm (44 %) (chi-squa
p
= 0.019). In patients with prior chemotherapy a benefit was indicated in those with a KPS ≥ 80.
Data on time to worsening of neurological status favoured TMZ over procarbazine as did data on time
to worsening of performance status (decrease to a KPS of < 70 or a decrease by at least 30 points). The

median times to progression in these endpoints ranged from 0.7 to 2.1 months longer for TMZ than for
rocarbazine (log rank p = < 0.01 to 0.03).
Recurrent anaplastic astrocytoma
In a multicentre, prospective phase II trial evaluating the safety and efficacy of oral TMZ in the
treatment of patients with anaplastic astrocytoma at first relapse, the 6 month PFS was 46 %. Th
median PFS was 5.4 months. Median overall survival was 14.6 months. Response rate, based on the
central reviewer assessment, was 35 % (13 CR and 43 PR) for the intent-to-treat population (ITT)
n=162. In 43 patients stable disease was reported. The 6-month event-free survival for the ITT
population was 44 % with a median event-free survival of 4.6 m
onths, which was similar to the results
r the progression-free survival. For the eligible histology population, the efficacy results were similar.
gical objective response or maintaining progression-free status was strongly
ssociated with maintained or improved quality of life.
Oral TMZ has been studied in paediatric patients (age 3-18 years) with recurrent brainstem glioma or
regimen administered daily for 5 days every 28 days. Tolerance
TMZ is similar to adults.
5.2 Pharmacokinetic properties
TMZ is spontaneously hydrolyzed at physiologic pH primarily to the active species, 3-methyl-(triaze
1-yl)imidazole-4-carboxamide (MTIC). MTIC is spontaneously hydrolyzed to 5-amino-imidazole-4-
carboxamide (AIC), a known intermediate in purine and nucleic acid biosynthesis, and to
methylhydrazine, which is believed to be the
th
to the AUC o
o
active alkylating species. The cytotoxicity of MTIC is
ought to be primarily due to alkylation of DNA mainly at the O
6
and N
7
positions of guanine. Relative
f TMZ, the exposure to MTIC and AIC is ~ 2.4 % and 23 %, respectively.
In vivo
, the t
1/2
f MTIC was similar to that of TMZ, 1.8 hr.
After oral administration to adult patients, TMZ is absorbed rapidely, with peak concentrations reached
s early as 20 minutes post-administration (mean time between 0.5 and 1.5 hours). After oral
n of
14
C-labelled TMZ, mean faecal excretion of
14
C over 7 days post-dose was 0.8 %
dicationg complete absorption.
TMZ demonstrates low protein binding (10 % to 20 %), and thus it is not expected to interact with
highly protein-bound substances.
PET studies in humans and preclinical data suggest that TMZ crosses the blood-brain barrier rapidly and
he CSF. CSF penetration was confirmed in one patient; CSF exposure based on AUC of
MZ was approximately 30 % of that in plasma, which is consistent with animal data.
F
urine over 24 hours, and the remainder excreted as temozolomide acid, 5-aminoimidazole-4-
carboxamide (AIC) or unidentified
14
. The major route of C elimination is renal.
ollowing oral administration, approximately 5 % to 10 % of the dose is recovered unchanged in the
s increase in a dose-related manner. Plasma clearance, volume of distribution and
alf-life are independent of dose.
recurrent high grade astrocytoma, in a
to
The half-life (t
1/2
) in plasma is approximately 1.8 hours
Analysis of population-based pharmacokinetics of TMZ revealed that plasma TMZ clearance was
independent of age, renal function
or tobacco use. In a separate pharmacokinetic study, plasma
harmacokinetic profiles in patients with mild to moderate hepatic impairment were similar to those
P
was 1,000 mg/m
2
per cycle bot
aediatric patients had a higher AUC than adult patients; however, the maximum tolerated dose (MTD)
h in children and in adults.
5.3 Preclinical safety data
Single-cycle (5-day dosing, 23 days non-treatment), 3- and 6-cycle toxicity studies were conducted
rats and dogs. The primary targets of toxicity included the bone marrow, lymphoreticular system, testes,
the gastrointestinal tract and, at higher doses, which were lethal to 60 % to 100 % of rats and dogs
tested, degeneration of the retina occurred. Most of the toxicity showed evidence of reversibility, exc
for adverse events on the male reproductive system and retinal degeneration. However, becau
d
been observed in clinical studies, this finding was not considered to have clinical relevance.
se the
oses implicated in retinal degeneration were in the lethal dose range, and no comparable effect has
TMZ is an embryotoxic, teratogenic and genotoxic alkylating agent. TMZ is more toxic to the rat and
dog than to humans, and the clinical dose approximates the minimum lethal dose in rats and dogs. Dose
related reductions in leukocytes and platelets appear to be sensitive indicators of toxicity. A variety
neoplasms, including mammary carcinomas, keratocanthoma of the skin and basal cell adenoma were
observed in the 6-cycle rat study while no tumours or pre-neoplastic changes were evident in dog
studies.
tu
agent.
Rats appear to be particularly sensitive to oncogenic effects of TMZ, with the occurrence of first
mours within 3 months of initiating dosing. This latency period is very short even for an alkylating
esults of the Ames/salmonella and Human Peripheral Blood Lymphocyte (HPBL) chromosome
berration tests showed a positive mutagenicity response.
Capsule content
:
anhydrous lactose,
colloidal anhydrous silica,
glycolate type A,
Capsule shell
:
gelatin,
titanium dioxide (E 171),
sodium lauril sulfate,
ide (E 172)
Printing ink:
shellac,
propylene glycol,
purified water,
ammonium hydroxide,
potassium hydroxide,
black iron oxide (E 172).
p
observed in patients with normal hepatic function.
sodium starch
ta
stearic acid.
Do not store above 30 °C.
Store in the original bottle in order to protect from moisture.
ly closed.
Do not store above 30 °C.
6.5 Nature and contents of container
Type I amber glass bottles with polypropylene child-resistant closures containing 5 -or 20 hard capsules.
ne bottle.
Sachets are composed of linear low density polyethylene (innermost layer), aluminium and polyethylene
terephthalate.
E
The carton contains 5 or 20 hard caps
ach sachet contains 1 hard capsule and is dispensed in a cardboard carton.
ules, individually sealed in sachets.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
Capsules should not be opened. If a capsule becomes damaged, contact of the powder contents with skin
o
washed immediately and thoroughly with soap and water.
r mucous membrane must be avoided. If Temodal comes into contact with skin or mucosa, it should be
P
cupboard. Accidental ingestion can be lethal for children.
atients should be advised to keep capsules out of the reach and sight of children, preferably in a locked
ny unused product or waste material should be disposed of in accordance with local requirements.
KETING AUTHORISATION HOLDER
alle 73
-1180 Bruxelles
elgium
MARKETING AUTHORISATION NUMBER(S)
EU/1/98/096/003
EU/1/98/096/004
E
E
U/1/98/096/013
U/1/98/096/014
DATE OF FIRST AUTHORISATION
/RENEWAL OF THE AUTHORISATION
ate of first authorisation: 26 January 1999.
ate of last renewal: 26 January 2009
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
Agency (EMEA) http://www.emea.europa.eu/
NAME OF THE MEDICINAL PRODUCT
Temodal 100 mg hard capsules
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each hard capsule contains 100 mg temozolomide.
Excipient: Each hard capsule contains 175.7 mg of anhydrous lactose.
For a full list of excipients, see section 6.1.
The hard capsules have an opaque white body, an opaque pink cap, and are imprinted with black ink.
The cap is imprinted with “Temodal”. The body is imprinted with "100 mg", the Schering-Plough logo
and two stripes.
4.1 Therapeutic indications
Temodal hard capsules is indicated for the treatment of:
-
adult patients with newly-diagnosed glioblastoma multiforme concomitantly with radiotherapy
(RT) and subsequently as monotherapy treatment.
children from the age of three years, adolescents and adult patients with malignant glioma, such
as glioblastoma multiforme or anaplastic astrocytoma, showing recurrence or progression after
standard therapy.
4.2 Posology and method of administration
Temodal hard capsules should only be prescribed by physicians experienced in the oncological
treatment of brain tumours.
Anti-emetic therapy may be administered (see section 4.4).
Adult patients with newly-diagnosed glioblastoma multiforme
Temodal hard capsules is administered in combination with focal radiotherapy (concomitant phase)
followed by up to 6 cycles of temozolomide (TMZ) monotherapy (monotherapy phase).
Concomitant phase
TMZ is administered orally at a dose of 75 mg/m
2
daily for 42 days concomitant with focal radiotherapy
(60 Gy administered in 30 fractions). No dose reductionsare recommended, but delay or discontinuation
of TMZ administration should be decided weekly according to haematological and non-haematological
toxicity criteria. TMZ administration can be continued throughout the 42 day concomitant period (up to
49 days) if all of the following conditions are met:
-
absolute neutrophil count (ANC) ≥ 1.5 x 10
9
/l
-
thrombocyte count ≥ 100 x 10
9
/l
-
common toxicity criteria (CTC) non-haematological toxicity ≤ Grade 1 (except for alopecia, nausea
and vomiting).
During treatment a complete blood count should be obtained weekly. TMZ administration should be
temporarily interrupted or permanently discontinued during the concomitant phase according to the
haematological and non-haematological toxicity criteria as noted in Table 1.
Table 1. TMZ dosing interruption or discontinuation during
concomitant radiotherapy and TMZ
Absolute neutrophil count
≥ 0.5 and < 1.5 x 10
9
/l
CTC non-haematological toxicity
(except for alopecia, nausea,
vomiting)
a: Treatment with concomitant TMZ can be continued when all of the following conditions are met:
absolute neutrophil count ≥ 1.5
x 10
9
/l; thrombocyte count ≥ 100
x 10
9
/l; CTC non-haematological
toxicity ≤ Grade 1 (except for alopecia, nausea, vomiting).
Four weeks after completing the TMZ + RT concomitant phase, TMZ is administered for up to 6 cycles
of monotherapy treatment. Dose in Cycle 1 (monotherapy) is 150 mg/m
2
once daily for 5 days followed
by 23 days without treatment. At the start of Cycle 2, the dose is escalated to 200 mg/m
2
if the CTC non-
haematological toxicity for Cycle 1 is Grade ≤ 2 (except for alopecia, nausea and vomiting), absolute
neutrophil count (ANC) is ≥ 1.5 x 10
9
/l, and the thrombocyte count is ≥ 100 x 10
9
/l. If the dose was not
escalated at Cycle 2, escalation should not be done in subsequent cycles. Once escalated, the dose
remains at 200 mg/m
2
per day for the first 5 days of each subsequent cycle except if toxicity occurs.
Dose reductions and discontinuations during the monotherapy phase should be applied according to
Tables 2 and 3.
During treatment a complete blood count should be obtained on Day 22 (21 days after the first dose of
TMZ). The dose should be reduced or administration discontinued according to Table 3.
TMZ dose levels for monotherapy treatment
Reduction for prior toxicity
Dose during Cycles 2-6 in absence of toxicity


















Table 3. TMZ dose reduction or discontinuation during monotherapy treatment
Toxicity
Reduce TMZ by 1 dose
level
a
Absolute neutrophil count
CTC non-haematological Toxicity
(except for alopecia, nausea, vomiting)
CTC Grade 3
a: TMZ dose levels are listed in Table 2.
b: TMZ is to be discontinued if:
•
dose level -1 (100 mg/m
2
) still results in unacceptable toxicity
•
the same Grade 3 non-haematological toxicity (except for alopecia, nausea, vomiting) recurs after dose
reduction.
Adult and paediatric patients 3 years of age or older with recurrent or progressive malignant glioma
:
A treatment cycle comprises 28 days. In patients previously untreated with chemotherapy, TMZ is
administered orally at a dose of 200 mg/m
2
once daily for the first 5 days followed by a 23 day
treatment interruption (total of 28 days). In patients previously treated with chemotherapy, the initial
dose is 150 mg/m
2
once
daily, to be increased in the second cycle to 200 mg/m
2
once daily, for 5 days if
there is no haematological toxicity (see section 4.4)
In patients 3 years of age or older, TMZ is only to be used in recurrent or progressive malignant glioma.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children is very limited (see sections 4.4 and 5.1).
Patients with hepatic or renal impairment
The pharmacokinetics of TMZ were comparable in patients with normal hepatic function and in those
with mild or moderate hepaticimpairment. No data are available on the administration of TMZ in
patients with severe hepatic impairment (Child’s Class C) or with renalimpairment. Based on the
pharmacokinetic properties of TMZ, it is unlikely that dose reductions are required in patients with
severe hepatic impairment or any degree of renalimpairment. However, caution should be exercised
when TMZ is administered in these patients.
Based on a population pharmacokinetic analysis in patients 19-78 years of age, clearance of TMZ is not
affected by age. However, elderly patients (> 70 years of age) appear to be at increased risk of
neutropenia and thrombocytopenia (see section 4.4).
Temodal hard capsules should be administered in the fasting state.
The capsules must be swallowed whole with a glass of water and must not be opened or chewed.
If vomiting occurs after the dose is administered, a second dose should not be administered that day.
Hypersensitivity to the active substanceor to any of the excipients.








Hypersensitivity to dacarbazine (DTIC).
Severe myelosuppression (see section 4.4).
4.4 Special warnings and precautions for use
Pneumocystis carinii
pneumonia
Patients who received concomitant TMZ and RT in a pilot trial for the prolonged 42-day schedule were
shown to be at particular risk for developing
Pneumocystis carinii
pneumonia (PCP). Thus, prophylaxis
against PCP is required for all patients receiving concomitant TMZ and RT for the 42-day regimen
(with a maximum of 49 days) regardless of lymphocyte count. If lymphopenia occurs, they are to
continue the prophylaxis until recovery of lymphopenia to grade ≤ 1.
There may be a higher occurrence of PCP when TMZ is administered during a longer dosing regimen.
However, all patients receiving TMZ, particularly patients receiving steroids, should be observed
closely for the development of PCP, regardless of the regimen.
Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukaemia, have
also been reported very rarely (see section 4.8).
Nausea and vomiting are very commonly associated with TMZ.
Anti-emetic therapy may be administered prior to or following administration of TMZ.
Adult patients with newly-diagnosed glioblastoma multiforme
Anti-emetic prophylaxis is recommended prior to the initial dose of concomitant phase and it is strongly
recommended during the monotherapy phase.
Patients with recurrent or progressive malignant glioma
Patients who have experienced severe (Grade 3 or 4) vomiting in previous treatment cycles may require
anti-emetic therapy.
Prior to dosing, the following laboratory parameters must be met: ANC ≥ 1.5 x 10
9
/l and platelet count
≥ 100 x 10
9
/l. A complete blood count should be obtained on Day 22 (21 days after the first dose) or
within 48 hours of that day, and weekly until ANC > 1.5 x 10
9
/l and platelet count > 100 x 10
9
/l. If
ANC falls to < 1.0 x 10
9
/l or the platelet count is < 50 x 10
9
/l during any cycle, the next cycle should be
reduced one dose level (see section 4.2). Dose levels include 100 mg/m
2
, 150 mg/m
2
, and 200 mg/m
2
.
The lowest recommended dose is 100 mg/m
2
.
There is no clinical experience with use of TMZ in children under the age of 3 years. Experience in
older children and adolescents is very limited (see sections 4.2 and 5.1).
Elderly patients (> 70 years of age)
Elderly patients appear to be at increased risk of neutropenia and thrombocytopenia, compared with
younger patients. Therefore, special care should be taken when TMZ is administered in elderly patients.
Men being treated with TMZ should be advised not to father a child up to 6 months after receiving the
last dose and to seek advice on cryoconservation of sperm prior to treatment (see section 4.6).
This medicinal product contains lactose. Patients with rare hereditary problems of galactose intolerance,
the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
4.5 Interaction with other medicinal products and other forms of interaction
Interaction studies have only been performed in adults.
In a separate phase I study, administration of TMZ with ranitidine did not result in alterations in the
extent of absorption of temozolomide or the exposure to its active metabolite monomethyl
triazenoimidazole carboxamide (MTIC).
Administration of TMZ with food resulted in a 33 % decrease in C
max
and a 9 % decrease in area under
the curve (AUC).
As it cannot be excluded that the change in C
max
is clinically significant, Temodal should be
administered without food.
Based on an analysis of population pharmacokinetics in phase II trials, co-administration of
dexamethasone, prochlorperazine, phenytoin, carbamazepine, ondansetron, H
2
receptor antagonists, or
phenobarbital did not alter the clearance of TMZ. Co-administration with valproic acid was associated
with a small but statistically significant decrease in clearance of TMZ.
No studies have been conducted to determine the effect of TMZ on the metabolism or elimination of
other medicinal products. However, since TMZ does not undergo hepatic metabolism and exhibits low
protein binding, it is unlikely that it would affect the pharmacokinetics of other medicinal products (see
section 5.2).
Use of TMZ in combination with other myelosuppressive agents may increase the likelihood of
myelosuppression.
4.6 Pregnancy and lactation
There are no data in pregnant women. In preclinical studies in rats and rabbits receiving 150 mg/m
2
TMZ, teratogenicity and/or foetal toxicity were demonstrated (see section 5.3). Temodal hard capsules
should not be administered to pregnant women. If use during pregnancy must be considered, the patient
should be apprised of the potential risk to the foetus. Women of childbearing potential should be
advised to use effective contraception to avoid pregnancy while they are receiving TMZ.
pregnancy while they are receiving TMZ.
It is not known whether TMZ is excreted in human milk; thus, breast-feeding should be discontinued
while receiving treatment with TMZ.
TMZ can have genotoxic effects. Therefore, men being treated with it should be advised not to father a
child up to 6 months after receiving the last dose and to seek advice on cryoconservation of sperm prior
to treatment, because of the possibility of irreversible infertility due to therapy with TMZ.
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. The ability to
drive and use machines may be impaired in patients treated with TMZ due to fatigue and somnolence.
Clinical trial experience
In patients treated with TMZ, whether used in combination with RT or as monotherapy following RT
for newly-diagnosed glioblastoma multiforme, or as monotherapy in patients with recurrent or
progressive glioma, the reported very common adverse reactions were similar: nausea, vomiting,
constipation, anorexia, headache and fatigue. Convulsions were reported very commonly in the newly-
diagnosed glioblastoma multiforme patients receiving monotherapy, and rash was reported very
commonly in newly-diagnosed glioblastoma multiforme patients receiving TMZ concurrent with RT
and also as monotherapy, and commonly in recurrent glioma. Most haematologic adverse reactions were
reported commonly or very commonly in both indications (Tables 4 and 5);the frequency of grade 3-4
laboratory findings is presented after each table.
In the tables undesirable effects are classified according to System Organ Class and frequency.
Frequency groupings are defined according to the following convention: Very common (≥ 1/10);
Common (≥ 1/100 to < 1/10); Uncommon (≥ 1/1,000 to < 1/100). Within each frequency grouping,
undesirable effects are presented in order of decreasing seriousness.
Newly-diagnosed glioblastoma multiforme
Table 4 provides treatment-emergent adverse events in patients with newly-diagnosed glioblastoma
multiforme during the concomitant and monotherapy phases of treatment.
Table 4. Treatment-emergent events during concomitant and monotherapy treatment phases
in patients with newly-diagnosed glioblastoma multiforme
TMZ + concomitant RT
n=288*
Infections and infestations
Common:
Infection
, Herpes
simplex
, wound
infection, pharyngitis, candidiasis oral
Infection, candidiasis oral
Herpes simplex
, herpes zoster,
influenza–like symptoms
Blood and lymphatic system disorders
Common:
Neutropenia, thrombocytopenia,
lymphopenia, leukopenia
Febril neutropenia,
thrombocytopenia, anaemia,
leukopenia
Febrile neutropenia, anaemia
Endocrine disorders
Uncommon:
Metabolism and nutrition disorders
Hyperglycaemia, weight decreased
Hypokalemia, alkaline phosphatase
increased, weight increased
Hyperglycaemia, weight increased















Psychiatric disorders
Common:
Anxiety, emotional lability, insomnia
Anxiety, depression, emotional
lability, insomnia
Agitation, apathy, behaviour disorder,
depression, hallucination
Nervous system disorders
Very common:
Convulsions, consciousness decreased,
somnolence, aphasia, balance impaired,
dizziness, confusion, memory
impairment, concentration impaired,
neuropathy, paresthesia, speech disorder,
tremor
Hemiparesis, aphasia, balance
impaired, somnolence, confusion,
dizziness, memory impairment,
concentration impaired, dysphasia,
neurological disorder (NOS),
neuropathy, peripheral neuropathy,
paresthesia, speech disorder, tremor
Status epilepticus, extrapyramidal
disorder, hemiparesis, ataxia, cognition
impaired, dysphasia, gait abnormal,
hyperesthesia, hypoesthesia, neurological
disorder (NOS), peripheral neuropathy
Hemiplegia, ataxia, coordination
abnormal, gait abnormal,
hyperesthesia, sensory disturbance
Visual field defect, vision blurred,
diplopia
Hemianopia, visual acuity reduced, vision
disorder, visual field defect, eye pain
Visual acuity reduced, eye pain, eyes
dry
Ear and labyrinth disorders
Hearing impairment, tinnitus
Otitis media, tinnitus, hyperacusis,
earache
Deafness, vertigo, earache
Haemorrhage, oedema, oedema leg
Haemorrhage, deep venous
thrombosis, oedema leg
Cerebral haemorrhage, hypertension
Embolism pulmonary, oedema,
oedema peripheral
Respiratory, thoracic and mediastinal disorders
Pneumonia, upper respiratory infection,
nasal congestion
Pneumonia, sinusitis, upper
respiratory infection, bronchitis
Gastrointestinal disorders
Constipation, nausea, vomiting
Constipation, nausea, vomiting


























Stomatitis, diarrhoea, abdominal pain,
dyspepsia, dysphagia
Stomatitis, diarrhoea, dyspepsia,
dysphagia, mouth dry
Abdominal distension, fecal
incontinence, gastrointestinal disorder
(NOS), gastroenteritis, haemorrhoids
Skin and subcutaneous tissue disorders
Very common:
Dermatitis, dry skin, erythema, pruritus
Skin exfoliation, photosensitivity
reaction, pigmentation abnormal
Erythema, pigmentation abnormal,
sweating increased
Musculoskeletal and connective tissue disorders
Common:
Muscle weakness, arthralgia
Muscle weakness, arthralgia,
musculoskeletal pain, myalgia
Myopathy, back pain, musculoskeletal
pain, myalgia
Renal and urinary disorders
Micturition frequency, urinary
incontinence
Reproductive system and breast disorders
Uncommon:
Vaginal haemorrhage, menorrhagia,
amenorrhea, vaginitis, breast pain
General disorders and administration site conditions
Very common:
Allergic reaction, fever, radiation injury,
face oedema, pain, taste perversion
Allergic reaction, fever, radiation
injury, pain, taste perversion
Asthenia, flushing, hot flushes, condition
aggravated, rigors, tongue discolouration,
parosmia, thirst
Asthenia, face oedema, pain,
condition aggravated, rigors, tooth
disorder, taste perversion
Hepatic enzymes increased, Gamma GT
increased, AST increased
*A patient who was randomised to the RT arm only, received TMZ + RT.
Myelosuppression (neutropenia and thrombocytopenia), which is known dose-limiting toxicity for most
cytotoxic agents, including TMZ, was observed. When laboratory abnormalities and adverse events
were combined across concomitant and monotherapy treatment phases, Grade 3 or Grade 4 neutrophil
























abnormalities including neutropenic events were observed in 8 % of the patients. Grade 3 or Grade 4
thrombocyte abnormalities, including thrombocytopenic events were observed in 14 % of the patients
who received TMZ.
Recurrent or progressive malignant glioma
In clinical trials, the most frequently occurring treatment-related undesirable effects were
gastrointestinal disorders, specifically nausea (43 %) and vomiting (36 %). These reactions were usually
Grade 1 or 2 (0 – 5 episodes of vomiting in 24 hours) and were either self-limiting or readily controlled
with standard anti-emetic therapy. The incidence of severe nausea and vomiting was 4 %.
Table 5 includes adverse reactions reported during clinical trials for recurrent or progressive malignant
glioma and following the marketing of Temodal.
Table 5. Adverse reactions in patients with recurrent or progressive malignant glioma
Infections and infestations
Rare:
Opportunistic infections, including PCP
Blood and lymphatic system disorders
Very common:
Neutropenia or lymphopenia (grade 3-4),
thrombocytopenia (grade 3-4)
Pancytopenia, anaemia (grade 3-4), leukopenia
Metabolism and nutrition disorders
Very common:
Nervous system disorders
Very common:
Somnolence, dizziness, paresthesia
Respiratory, thoracic and mediastinal disorders
Common:
Gastrointestinal disorders
Very common:
Vomiting, nausea, constipation
Diarrhoea, abdominal pain, dyspepsia
Skin and subcutaneous tissue disorders
Common:
Erythema multiforme, erythroderma, urticaria,
exanthema
General disorders and administration site conditions
Very common:
Fever, asthenia, rigors, malaise, pain, taste perversion
Allergic reactions, including anaphylaxis, angioedema
Grade 3 or 4 thrombocytopenia and neutropenia occurred in 19 % and 17 % respectively, of patients
treated for malignant glioma. This led to hospitalisation and/or discontinuation of TMZ in 8 % and 4 %,
respectively. Myelosuppression was predictable (usually within the first few cycles, with the nadir
between Day 21 and Day 28), and recovery was rapid, usually within 1-2 weeks. No evidence of
cumulative myelosuppression was observed. The presence of thrombocytopenia may increase the risk of
bleeding, and the presence of neutropenia or leukopenia may increase the risk of infection.


























In a population pharmacokinetics analysis of clinical trial experience there were 101 female and
169 male subjects for whom nadir neutrophil counts were available and 110 female and 174 male
subjects for whom nadir platelet counts were available. There were higher rates of Grade 4 neutropenia
(ANC < 0.5 x 10
9
/l), 12 %
vs
5 %, and thrombocytopenia (< 20 x 10
9
/l ), 9 %
vs
3 %, in women
vs
men
in the first cycle of therapy. In a 400 subject recurrent glioma data set, Grade 4 neutropenia occurred in
8 % of female
vs
4 % of male subjects and Grade 4 thrombocytopenia in 8 % of female
vs
3 % of male
subjects in the first cycle of therapy. In a study of 288 subjects with newly-diagnosed glioblastoma
multiforme, Grade 4 neutropenia occurred in 3 % of female
vs
0 % of male subjects and Grade 4
thrombocytopenia in 1 % of female
vs
0 % of male subjects in the first cycle of therapy.
Post-Marketing Experience
Antineoplastic agents, and notably alkylating agents, have been associated with a potential risk of
myelodysplastic syndrome (MDS) and secondary malignancies, including leukaemia. Very rare cases of
MDS and secondary malignancies, including myeloid leukaemia have been reported in patients treated
with regimens that included TMZ. Prolonged pancytopenia, which may result in aplastic anaemia has
been reported very rarely
.
Cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported very rarely.
Cases of interstitial pneumonitis/pneumonitis have been reported very rarely.
Doses of 500, 750, 1,000, and 1,250 mg/m
2
(total dose per cycle over 5 days) have been evaluated
clinically in patients. Dose-limiting toxicity was haematological and was reported with any dose but is
expected to be more severe at higher doses. An overdose of 10,000 mg (total dose in a single cycle, over
5 days) was taken by one patient and the adverse reactions reported were pancytopenia, pyrexia, multi-
organ failure and death. There are reports of patients who have taken the recommended dose for more
than 5 days of treatment (up to 64 days) with adverse events reported including bone marrow
suppression, with or without infection, in some cases severe and prolonged and resulting in death. In the
event of an overdose, haematological evaluation is needed. Supportive measures should be provided as
necessary.
PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic properties
Pharmacotherapeutic group:
Antineoplastic agents - Other alkylating agents, ATC code: L01A X03
Temozolomide is a triazene, which undergoes rapid chemical conversion at physiologic pH to the active
monomethyl triazenoimidazole carboxamide (MTIC). The cytotoxicity of MTIC is thought to be due
primarily to alkylation at the O
6
position of guanine with additional alkylation also occurring at the N
7
position. Cytotoxic lesions that develop subsequently are thought to involve aberrant repair of the
methyl adduct.
Newly-diagnosed glioblastoma multiforme
A total of 573 patients were randomised to receive either TMZ + RT (n=287) or RT alone (n=286).
Patients in the TMZ + RT arm received concomitant TMZ (75 mg/m
2
) once daily, starting the first day
of RT until the last day of RT, for 42 days (with a maximum of 49 days). This was followed by
monotherapy TMZ (150 - 200 mg/m
2
) on Days 1 - 5 of every 28-day cycle for up to 6 cycles, starting
4 weeks after the end of RT. Patients in the control arm received RT only.
Pneumocystis carinii
pneumonia (PCP) prophylaxis was required during RT and combined TMZ therapy.
TMZ was administered as salvage therapy in the follow-up phase in 161 patients of the 282 (57 %) in
the RT alone arm, and 62 patients of the 277 (22 %) in the TMZ + RT arm.
The hazard ratio (HR) for overall survival was 1.59 (95 % CI for HR=1.33 -1.91) with a log-rank
p < 0.0001 in favour of the TMZ arm. The estimated probability of surviving 2 years or more (26 %
vs
10 %) is higher for the RT + TMZ arm. The addition of concomitant TMZ to RT, followed by TMZ
monotherapy in the treatment of patients with newly-diagnosed glioblastoma multiforme demonstrated a
statistically significant improvement in overall survival (OS) compared with RT alone (Figure 1).
HR (95% C.I.) = 1.59 (1.33 – 1.91)
log-rank p-value < .0001
Kaplan-Meier curves for overall survival (intent-to-treat population)
The results from the trial were not consistent in the subgroup of patients with a poor performance status
(WHO PS=2, n=70), where overall survival and time to progression were similar in both arms.
However, no unacceptable risks appear to be present in this patient group.
Recurrent or progressive malignant glioma
Data on clinical efficacy in patients with glioblastoma multiforme (Karnofsky performance status [KPS]
≥ 70), progressive or recurrent after surgery and RT, were based on two clinical trials with oral TMZ.
One was a non-comparative trial in 138 patients (29 % received prior chemotherapy), and the other was
a randomised active-controlled trial of TMZ
vs
procarbazine in a total of 225 patients (67 % received
prior treatment with nitrosourea based chemotherapy). In both trials, the primary endpoint was
progression-free survival (PFS) defined by MRI scans or neurological worsening. In the non-
comparative trial, the PFS at 6 months was 19 %, the median progression-free survival was 2.1 months,
and the median overall survival 5.4 months. The objective response rate (ORR) based on MRI scans was
8 %.
In the randomised active-controlled trial, the PFS at 6 months was significantly greater for TMZ than for
procarbazine (21 %
vs
8 %, respectively – chi-square p = 0.008) with median PFS of 2.89 and
1.88 months respectively (log rank p = 0.0063). The median survival was 7.34 and 5.66 months for TMZ
and procarbazine, respectively (log rank p = 0.33). At 6 months, the fraction of surviving patients was
significantly higher in the TMZ arm (60 %) compared with the procarbazine arm (44 %) (chi-square
p = 0.019). In patients with prior chemotherapy a benefit was indicated in those with a KPS ≥ 80.
Data on time to worsening of neurological status favoured TMZ over procarbazine as did data on time
to worsening of performance status (decrease to a KPS of < 70 or a decrease by at least 30 points). The
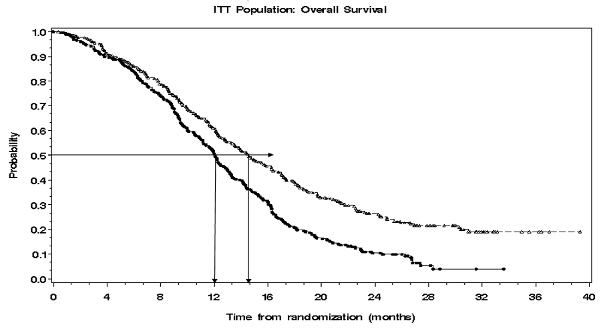

median times to progression in these endpoints ranged from 0.7 to 2.1 months longer for TMZ than for
procarbazine (log rank p = < 0.01 to 0.03).
Recurrent anaplastic astrocytoma
In a multicentre, prospective phase II trial evaluating the safety and efficacy of oral TMZ in the
treatment of patients with anaplastic astrocytoma at first relapse, the 6 month PFS was 46 %. The
median PFS was 5.4 months. Median overall survival was 14.6 months. Response rate, based on the
central reviewer assessment, was 35 % (13 CR and 43 PR) for the intent-to-treat population (ITT)
n=162. In 43 patients stable disease was reported. The 6-month event-free survival for the ITT
population was 44 % with a median event-free survival of 4.6 months, which was similar to the results
for the progression-free survival. For the eligible histology population, the efficacy results were similar.
Achieving a radiological objective response or maintaining progression-free status was strongly
associated with maintained or improved quality of life.
Oral TMZ has been studied in paediatric patients (age 3-18 years) with recurrent brainstem glioma or
recurrent high grade astrocytoma, in a regimen administered daily for 5 days every 28 days. Tolerance
to TMZ is similar to adults.
5.2 Pharmacokinetic properties
TMZ is spontaneously hydrolyzed at physiologic pH primarily to the active species, 3-methyl-(triazen-
1-yl)imidazole-4-carboxamide (MTIC). MTIC is spontaneously hydrolyzed to 5-amino-imidazole-4-
carboxamide (AIC), a known intermediate in purine and nucleic acid biosynthesis, and to
methylhydrazine, which is believed to be the active alkylating species. The cytotoxicity of MTIC is
thought to be primarily due to alkylation of DNA mainly at the O
6
and N
7
positions of guanine. Relative
to the AUC of TMZ, the exposure to MTIC and AIC is ~ 2.4 % and 23 %, respectively.
In vivo
, the t
1/2
of MTIC was similar to that of TMZ, 1.8 hr.
After oral administration to adult patients, TMZ is absorbed rapidely, with peak concentrations reached
as early as 20 minutes post-administration (mean time between 0.5 and 1.5 hours). After oral
administration of
14
C-labelled TMZ, mean faecal excretion of
14
C over 7 days post-dose was 0.8 %
indicationg complete absorption.
TMZ demonstrates low protein binding (10 % to 20 %), and thus it is not expected to interact with
highly protein-bound substances.
PET studies in humans and preclinical data suggest that TMZ crosses the blood-brain barrier rapidly and
is present in the CSF. CSF penetration was confirmed in one patient; CSF exposure based on AUC of
TMZ was approximately 30 % of that in plasma, which is consistent with animal data.
The half-life (t
1/2
) in plasma is approximately 1.8 hours. The major route of
14
C elimination is renal.
Following oral administration, approximately 5 % to 10 % of the dose is recovered unchanged in the
urine over 24 hours, and the remainder excreted as temozolomide acid, 5-aminoimidazole-4-
carboxamide (AIC) or unidentified polar metabolites.
Plasma concentrations increase in a dose-related manner. Plasma clearance, volume of distribution and
half-life are independent of dose.
Analysis of population-based pharmacokinetics of TMZ revealed that plasma TMZ clearance was
independent of age, renal function
or tobacco use. In a separate pharmacokinetic study, plasma
pharmacokinetic profiles in patients with mild to moderate hepatic impairment were similar to those
observed in patients with normal hepatic function.
Paediatric patients had a higher AUC than adult patients; however, the maximum tolerated dose (MTD)
was 1,000 mg/m
2
per cycle both in children and in adults.
5.3 Preclinical safety data
Single-cycle (5-day dosing, 23 days non-treatment), 3- and 6-cycle toxicity studies were conducted in
rats and dogs. The primary targets of toxicity included the bone marrow, lymphoreticular system, testes,
the gastrointestinal tract and, at higher doses, which were lethal to 60 % to 100 % of rats and dogs
tested, degeneration of the retina occurred. Most of the toxicity showed evidence of reversibility, except
for adverse events on the male reproductive system and retinal degeneration. However, because the
doses implicated in retinal degeneration were in the lethal dose range, and no comparable effect has
been observed in clinical studies, this finding was not considered to have clinical relevance.
TMZ is an embryotoxic, teratogenic and genotoxic alkylating agent. TMZ is more toxic to the rat and
dog than to humans, and the clinical dose approximates the minimum lethal dose in rats and dogs. Dose-
related reductions in leukocytes and platelets appear to be sensitive indicators of toxicity. A variety of
neoplasms, including mammary carcinomas, keratocanthoma of the skin and basal cell adenoma were
observed in the 6-cycle rat study while no tumours or pre-neoplastic changes were evident in dog
studies. Rats appear to be particularly sensitive to oncogenic effects of TMZ, with the occurrence of first
tumours within 3 months of initiating dosing. This latency period is very short even for an alkylating
agent.
Results of the Ames/salmonella and Human Peripheral Blood Lymphocyte (HPBL) chromosome
aberration tests showed a positive mutagenicity response.
PHARMACEUTICAL PARTICULARS
Capsule content
:
anhydrous lactose,
colloidal anhydrous silica,
sodium starch glycolate type A,
tartaric acid,
stearic acid.
Capsule shell
:
gelatin,
titanium dioxide (E 171),
sodium lauril sulfate,
red iron oxide (E172).
Printing ink:
shellac,
propylene glycol,
purified water,
ammonium hydroxide,
potassium hydroxide,
black iron oxide (E 172).
6.4 Special precautions for storage
Do not store above 30 °C.
Store in the original bottle in order to protect from moisture.
Keep the bottle tightly closed.
Do not store above 30 °C.
6.5 Nature and contents of container
Type I amber glass bottles with polypropylene child-resistant closures containing 5 -or 20 hard capsules.
The carton contains one bottle.
Sachets are composed of linear low density polyethylene (innermost layer), aluminium and polyethylene
terephthalate.
Each sachet contains 1 hard capsule and is dispensed in a cardboard carton.
The carton contains 5 or 20 hard capsules, individually sealed in sachets.
Not all pack sizes may be marketed.
6.6 Special precautions for disposal and other handling
Capsules should not be opened. If a capsule becomes damaged, contact of the powder contents with skin
or mucous membrane must be avoided. If Temodal comes into contact with skin or mucosa, it should be
washed immediately and thoroughly with soap and water.
Patients should be advised to keep capsules out of the reach and sight of children, preferably in a locked
cupboard. Accidental ingestion can be lethal for children.
Any unused product or waste material should be disposed of in accordance with local requirements.
MARKETING AUTHORISATION HOLDER
SP Europe
Rue de Stalle 73
B-1180 Bruxelles
Belgium
MARKETING AUTHORISATION NUMBER(S)
EU/1/98/096/005
EU/1/98/096/006
EU/1/98/096/015
EU/1/98/096/016
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 26 January 1999.
Date of last renewal: 26 January 2009
10. DATE OF REVISION OF THE TEXT
Detailed information on this medicinal product is available on the website of the European Medicines
The active substance is temozolomide. Each vial contains 100 mg temozolomide. After reconstitution,
each ml solution for infusion contains 2.5 mg of temozolomide.
The other ingredients are mannitol (E421), threonine, polysorbate 80, sodium citrate (for
pH-adjustment) and hydrochloric acid concentrated (for pH-adjustment).
What Temodal looks like and contents of the pack
The powder for solution for infusion is a white powder. Temodal is available in a glass vial, with a butyl
rubber stopper and aluminium seal with a flip-off bonnet.
Each pack contains 1 vial of 100 mg temozolomide.
Marketing Authorization Holder and Manufacturer
Marketing Authorisation Holder: SP Europe, Rue de Stalle 73, B-1180 Bruxelles, Belgium
Manufacturer: SP Labo N.V., Industriepark 30, B-2220 Heist-op-den-Berg, Belgium
For any information about this medicinal product, please contact the local representative of the
Marketing Authorisation Holder:
België/Belgique/Belgien
Rue de Stalle/Stallestraat 73
B-1180 Bruxelles/Brussel/Brüssel
Tél/Tel: + 32-(0)2 370 92 11
Luxembourg/Luxemburg
Rue de Stalle 73
B-1180 Bruxelles/Brüssel
Belgique/Belgien
Tél/Tel: + 32-(0)2 370 92 11
България
Ийст Парк Трейд Център
Бул. „Н.Й.Вапцаров” 53А, ет. 2
BG-София 1407
Тел.: +359 2 806 3030
Magyarország
Alkotás u. 53.
H-1123 Budapest
Tel.: +36 1 457-8500
Česká republika
Ke Štvanici 3
CZ-186 00 Praha 8
Tel: +420 221771250
Malta
168 Christopher Street
MT-VLT02 Valletta
Tel: + 356-21 23 21 75
Danmark
Lautrupbjerg 2
DK-2750 Ballerup
Tlf: + 45-44 39 50 00
Nederland
Waarderweg 39
NL-2031 BN Haarlem
Tel: + 31-(0)800 9999000
Deutschland
Thomas-Dehler-Straße 27
D-81737 München
Tel: + 49-(0)89 627 31-0
Norge
Pb. 398
N-1326 Lysaker
Tlf: + 47 67 16 64 50
Eesti
Järvevana tee 9
EE-11314 Tallinn
Tel: + 372 654 96 86
Österreich
Am Euro Platz 2
A-1120 Wien
Tel: +43-(0) 1 813 12 31
Ελλάδα
Αγίου Δημητρίου 63
GR-174 55 Άλιμος
Tηλ.: + 30-210 98 97 300
Polska
Ul. Taśmowa 7
PL-02-677 Warszawa
Tel.: + 48-(0)22 478 41 50
España
Josefa Valcárcel, 38
E-28027 Madrid
Tel: + 34-91 321 06 00
Portugal
Rua Agualva dos Açores 16
P-2735-557 Agualva-Cacém
Tel: +351-21 433 93 00
France
34 avenue Léonard de Vinci
F-92400 Courbevoie
Tél: + 33-(0)1 80 46 40 40
România
Şos. Bucureşti-Ploieşti, nr. 17-21,
Băneasa Center, et. 8, sector 1
RO-013682 Bucureşti
Tel: + 40 21 233 35 30
Shire Park
Welwyn Garden City
Hertfordshire AL7 1TW
Tel: +44-(0)1 707 363 636
Dunajska 22
SI-1000 Ljubljana
Tel: + 386 01 3001070
Ísland
Hörgatún 2
IS-210 Garðabær
Sími: + 354 535 70 00
Slovenská republika
Strakova 5
SK-811 01 Bratislava
Tel: + 421 (2) 5920 2712
Italia
Via fratalli Cervi snc,
Centro Direzionale Milano Due
Palazzo Borromini
I-20090 Segrate (Milano)
Tel: + 39-02 21018.1
Suomi/Finland
PL 46/PB 46
FIN-02151 Espoo/Esbo
Puh/Tel: + 358 (0)9 804 650
Κύπρος
Οδός Αγίου Νικολάου, 8
CY-1055 Λευκωσία
Τηλ: +357-22 757188
Sverige
Box 7125
S-192 07 Sollentuna
Tel: + 46-(0)8 6261400
Latvija
Bauskas 58a -401
Rīga, LV-1004
Tel: + 371-7 21 38 25
United Kingdom
Shire Park
Welwyn Garden City
Hertfordshire AL7 1TW - UK
Tel: + 44-(0)1 707 363 636
Lietuva
Kęstučio g. 65/40
LT-08124 Vilnius
Tel. + 370 52 101868
This leaflet was last approved on
Detailed information on this medicinal product is available on the website of the European Medicines
The following information is intended for medical or health care professional use only:
Caution must be exercised in handling Temodal 2.5 mg/ml powder for solution for infusion. The use of
gloves and aseptic technique is required. If Temodal 2.5 mg/ml comes into contact with skin or mucosa,
it should be washed immediately and thoroughly with soap and water.
Each vial must be reconstituted with 41 ml sterilised water for injections. The resulting solution contains
2.5 mg/ml TMZ. The vials should be gently swirled and not shaken. The solution should be inspected
and any vial containing visible particulate matter should not be used. Reconstituted product must be
used within 14 hours, including infusion time.
A volume up to 40 ml reconstituted solution should be withdrawn, according to the total prescribed dose
and transferred into an empty 250 ml PVC infusion bag. Studies with non-PVC bags have not been
conducted. The pump tubing should be attached to the bag, the tubing purged and then capped. Temodal
2.5 mg/ml must be administered by intravenous infusion
only
over a period of 90 minutes.
In absence of compatibility studies this medicinal product must not be mixed with other medicinal
products or infused simultaneously through the same intravenous line.
This medicinal product is for single use only. Any unused product or waste material should be disposed
of in accordance with local requirements.
Source: European Medicines Agency
 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).
- If you wish to link to this page, you can do so by referring to the URL address below this line.
https://theodora.com/drugs/eu/temodal.html
Copyright © 1995-2021 ITA all rights reserved.
|























































































































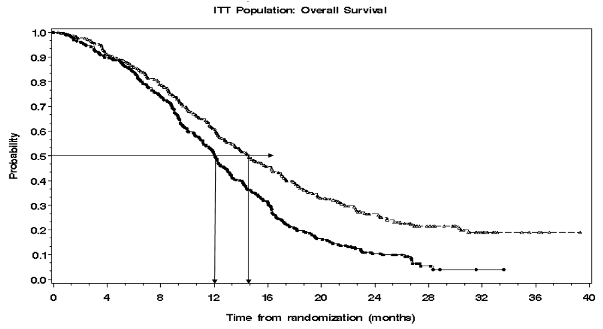




















































































































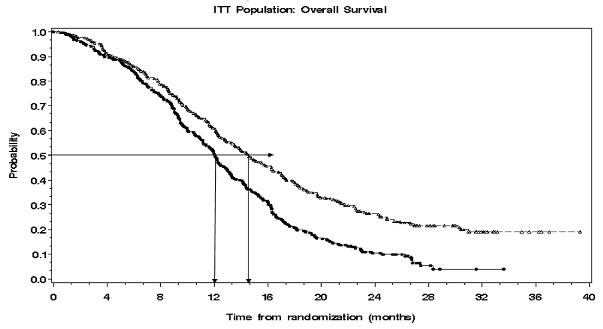






















































































































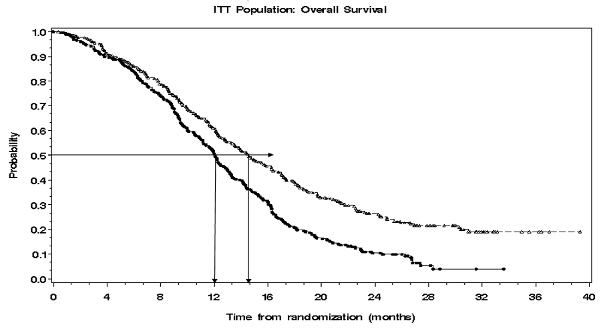

 - Please bookmark this page (add it to your favorites).
- Please bookmark this page (add it to your favorites).










































